|
Adapted from Katie Januszewicz's Grand Rounds lecture August 30th, 2017 Inflammation of the pancreas can be limited to mild inflammation to severe necrosis of the pancreas and surrounding tissue. Most cases (80%) involve only mild inflammation, however severe pancreatitis can lead to a 30% mortality rate. Most cases are secondary to gallstones or alcohol, but up to 5% of ERCP patients present with post-procedure pancreatitis. Additionally, many medications (120) can cause pancreatitis. In severe cases this can lead to inflammatory responses in nearby tissue and even systemically.
Pancreatitis occurs secondary to an unclear mechanism involving trypsin, a protease that is typically converted from pancreatic trypsinogen in the duodenum. When trypsin is activated in the pancreatic acinar cells, this continues unregulated leading to activation of other digestive enzymes and auto-digestion of the pancreas.
0 Comments
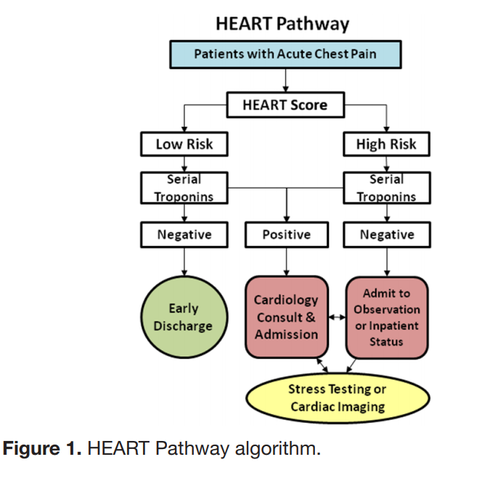
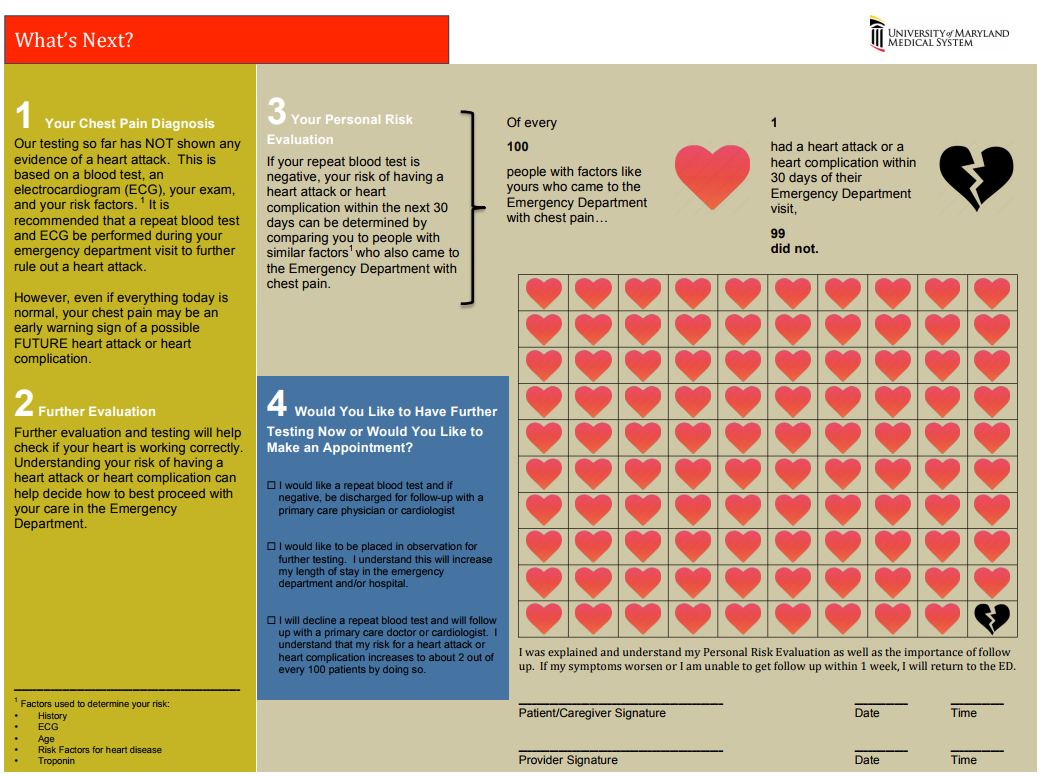
The “Delta Trop” is not a rule out test! It should be used in conjunction with the HEART score to have a conversation with the patient about risks/benefits of discharge vs admission during a low-risk chest pain evaluation. The “Delta Trop” refers to serial troponin testing, anywhere from 2 to 6 hours between the first and second troponin. As troponin testing has improved, the time between each test has been lowered. The most recent data recommends 3 hours between each troponin when the high-sensitivity test is used. The delta troponin is not a “Rule Out”; it is used in addition to the rest of the patient’s visit to help risk stratify them into low, moderate, or high risk chest pain. The HEART Pathway combines the patient’s HEART score with two serial troponins at zero and three hours. Observational studies showed 20% of patients with chest pain can be safely discharged utilizing this protocol, while maintaining a negative predictive value of Major Cardiac Event at >99%. This is actually a lower rate of MACE than the traditional HEART score alone (1.0% versus 1.7%). A recent controlled trial increased early discharges by 21.3%, decreased cardiac testing by 12.1%, and decreased length of stay by 12 hours! Just because we are discharging people, however, doesn’t mean they have been ‘ruled out’ for cardiac issues. Remember, 1% of those discharged had a major cardiac event within 30 days. The “Delta Trop” should be used as a shared decision making tool where the patient is provided the information and risks/benefits of admission versus discharge. Attached is the University of Maryland shared decision making tool, which is used in conjunction with a bedside discussion, to explain the risks and benefits.
Shared Decision MakingWhen you identify a patient with a low heart score (1-3) you can use this dotphrase to improve your documentation of your shared decision making conversation, and to make sure you are not forgetting alternative causes of chest pain. Remember, that by hitting “F3” your cursor will jump to the next “_” Patient HEART score 0-3, with risk of MACE 1.7% within 6 weeks, discussed with patient the potential for symptoms to be cardiac in nature and the need for follow up and return precautions. Other potential causes of the patient's presentation were considered; PERC _. Well's _. Pain not consistent with aortic etiology. Physical exam reassuring without signs of pneumothorax, pulmonary infection, heart failure exacerbation, or respiratory failure. Initial troponin negative. Discussed with patient the possibility of approximately 2% of an adverse cardiac event within the next 4-6 weeks, as well as options for further treatment, including observation admission, a second troponin at 3 hours, or discharge. After this discussion, the patient elected to _.
Pulmonary embolisms present with a broad variety of symptoms from chest pain to shortness of breath, and even fevers. Common exam findings include tachypnea and tachycardia. Risk factors include recent surgery, trauma, prolonged immobility, active cancer, birth control pills or hormone replacement therapy, or a history of prior embolism. Definitions
Pulmonary Embolism is the Arresting PatientPatients who arrest with a strong suspicion of pulmonary embolism may be treated with TPA. Bedside ultrasound should be used to help rule out alternative causes, such as tamponade or aortic dissection. Bedside ultrasound should also be used to evaluate for right heart strain prior to TPA.
The initial dose of TPA in a cardiac arrest varies depending on what study is being evaluated. Some doses include an initial bolus of 10-15mg of TPA followed by an influsion of 85-90mg over an hour. Local protocol calls for a single bolus of 50mg over 2 minutes in cardiac arrest. This should be followed by at least 15-20 additional minutes of CPR to allow for TPA to circulate. A second dose could be considered. Current data shows that there is no difference in outcome when comparing patients who do and do not receive TPA during cardiac arrest. The same data also does not show increased risk of severe bleeding when comparing these populations. Undifferentiated cardiac arrest is NOT an indication for TPA. Adapted from Dr. Brian D’Cruz’s Grand Round Lecture August 23, 2017 In addition to classical GI complaints such as giardia, tropical areas have the additional issues such as limited resources, lack of physicians, and potentially poorly treated water resources. Severe malnutrition and dehydration are common complaints.
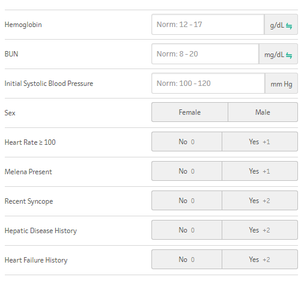
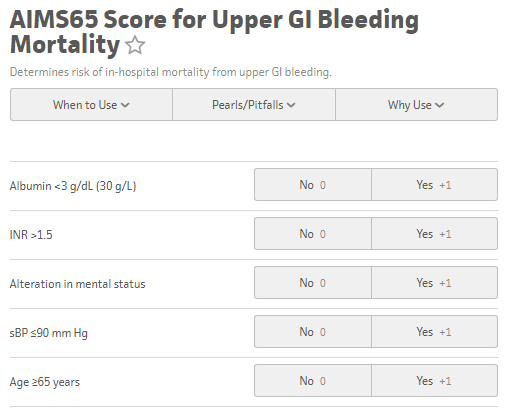
The GBS score can be utilized for upper GI bleeds to risk stratify patients for potential discharge from the emergency department, and was originally published in 2000 in the Lancet based off a Scottish study in 1997 and validated in 2007. The GBS classifies Low Risk as those patients with a score of Zero. Any score higher than zero is considered to potentially require intervention, transfusion, or endoscopy The AIM65 Score is a less complicated scoring system derived retrospectively in 2011 from a cohort of >29,000 patients.
Acetylcholinesterase inhibitors include carbamates, organophosphates, and chemical weapons, which bind to carboxylic esters, such as acetylcholinesterase at the nerve terminals and within RBCs. These are commonly used as pesticides, but have also been utilized as chemical weapons, such as the Tokyo subway poisoning in 1995 which utilized Sarin.
Additionally, many Alzheimer medications are also acetylcholinesterase inhibitors, and can give the same symptoms when at elevated amounts or overdose, and can present with vague or mild symptoms. |
Categories
Archive
February 2018
Please read our Terms of Use.
|
||||||||||||||