|
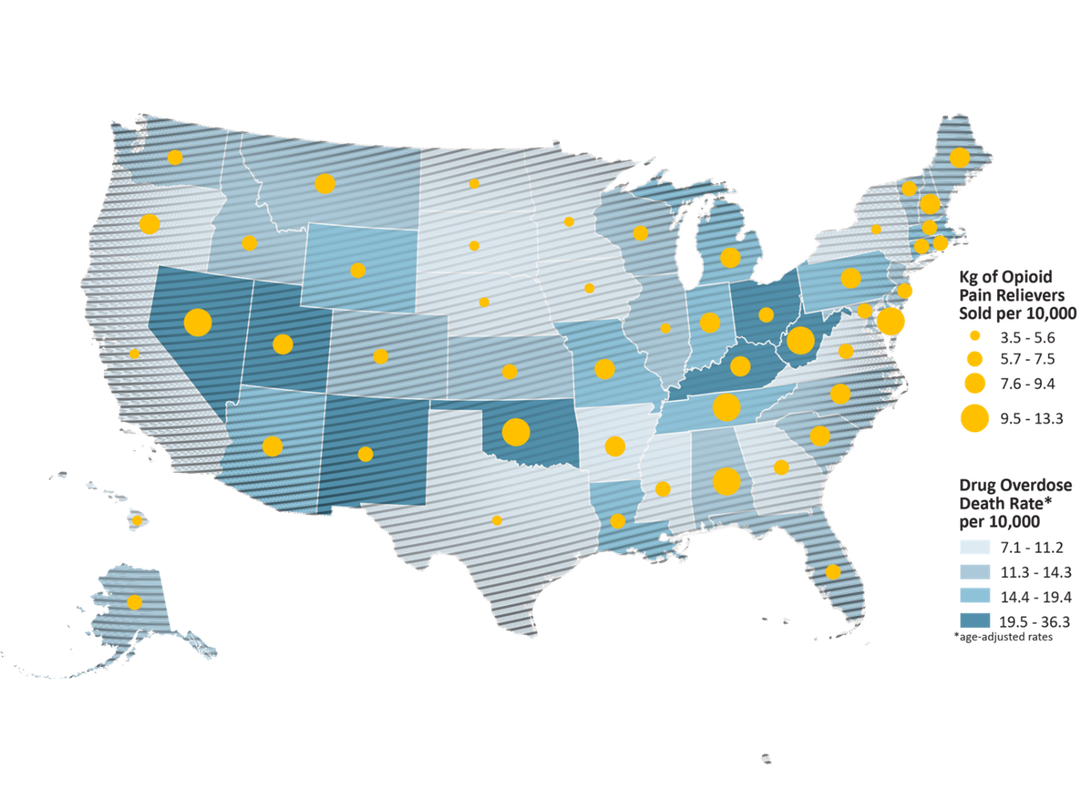
Adapted from Dr. Natalie Kirilichin's ACEP Physician Panel Opioid medications are frequently considered to be more powerful painkillers than many other alternatives, however the evidence shows they are actually less effective than many over-the-counter painkillers. Additionally, there are many side effects to opioid medications including the risk of addiction which has led to the current opioid epidemic. 20.8 million people in the US are living with a substance use disorder, and the largest contributor to drug overdoses is prescription painkillers. In some situations, limited use is appropriate, but for the broad majority of situations, opioids are not the best option available. It is also important for the medical community to address this inadequate and unsafe treatment of pain and change practice standards to guide care that is more appropriate for what our patients need and deserve. Despite the lack of evidence for opioid treatment, the use of opioids has exploded since the 1990's for many reasons. Primarily, pharmaceutical companies have done a good job marketing opioids, so many doctors have come to believe opioids are actually stronger than other medications, and marketing in the 1990's led practitioners to believe opioids had minimal addiction risk. In 2986, the WHO pain ladder was created by a panel of experts to recommend the best way to treat cancer pain. This recommends that practitioners use NSAIDs and acetaminophen for mild cancer pain but then change to weak or strong opioids for more severe pain, or if NSAIDs and acetaminophen are not effective. While many pain specialists reference the WHO pain ladder regarding effective treatment of pain, it is noteworthy that these recommendations are based on expert opinion (the weakest source of recommendation).
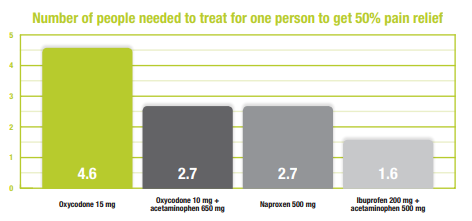
Acute and chronic pain is better relieved with nonopioidsAcute pain (<3 months) treatment strategy is significantly different than chronic pain (>3 months). Acute pain includes more of an emotional experience than chronic pain, which can be impacted by opioid medications. For this reason, acute pain is frequently treated with opioid medication, while the CDC recommends against opioids for most chronic pain. When evaluating the treatment of acute pain, ibuprofen, Tylenol, and naproxen all have a smaller number needed to treat than oxycodone to relieve pain. Additionally, opioid treatment can also cause hyperalgesa, or increased sensitivity to pain with prolonged use. National Level GuidelinesIn an effort to provide consistent opioid prescribing guidelines, the CDC released Guideline for Prescribing Opioids for Chronic Pain in 2016. The guidelines focus mainly on treatment of chronic pain, and these new recommendations focus on clinical practice and provide evidence and guidance to improve how these drugs are prescribed—and ultimately improve patient care. The CDC guidelines recommend starting with the lowest possible dose of opioids when used, and only for a short duration. Washington State PoliciesWashington State was one of the first states to adopt specific Emergency Department opioid prescribing guildlines, leading to decreased prescriptions and decreased medicare/medicaid costs. Their program, entitled ER is for Emergencies, started in 2014 and saved over $34 million in Medicaid fee-for-service emergency care costs.
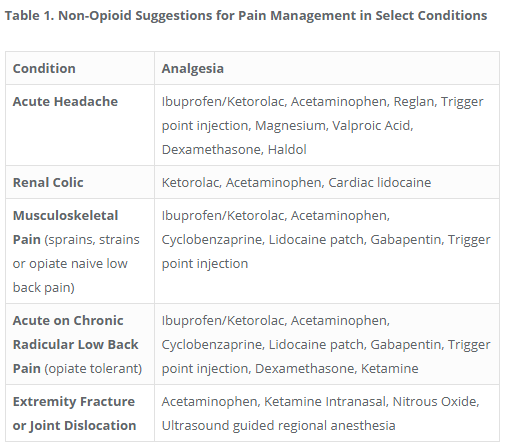
ALTO ProgramSt. Joseph’s Regional Medical Center in Paterson, New Jersey launched a formal program called Alternatives to Opiates (ALTO) to help improve pain management, patient care, and patient safety. The ALTO program uses targeted non-opioid pain management including medications, injections, nitrous-oxide, and nerve blocks to avoid opioid use whenever possible. The program identifies five specific conditions and provides specific alternatives to opioids for each condition. The original program reduced opiate use by 47%. The Colorado chapter of ACEP went even further, creating a 42 page guide to opioid use and prescribing guidelines (below).
0 Comments
Leave a Reply. |
Categories
Archive
February 2018
Please read our Terms of Use.
|
||||||||||||