|
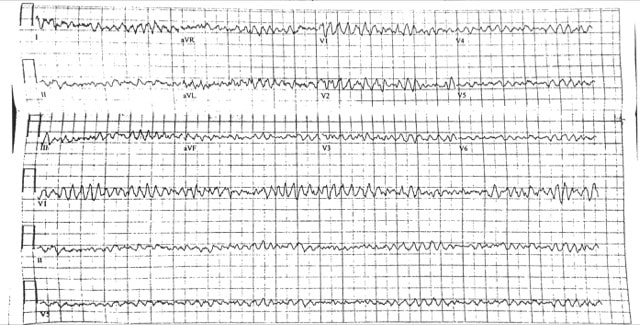
What is the diagnosis?
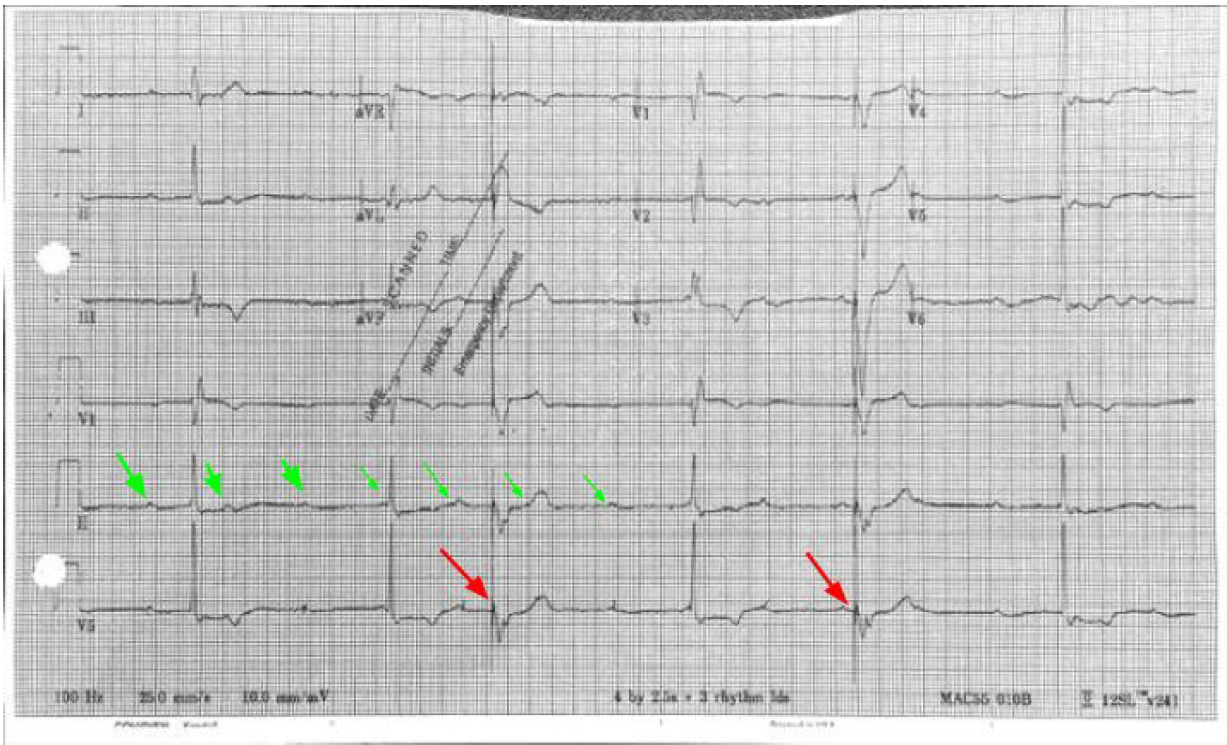
3rd Degree AV Block (Complete Heart Block) - Look at the rhythm strip and notice there is no relation between the P waves (Green Arrows) and QRS complexes which diagnoses 3rd Degree. It helps to get a piece of paper (calipers if you have) and measure the P waves. They can often be buried in the T wave or QRS complex. It is not 2nd Degree AV Block because both Mobitz I (progressively prolonged PR interval before dropped QRS) and Mobitz II (intermittent AV Block) will show some pattern of relation between the P wave and QRS complex. The escape rhythm is narrow and thus a junctional escape rhythm indicating the block is above the bundle of his. A wide complex would indicate a block at or below the bundle of His and ventricular escape rhythm. Name some possible etiologies
Etiologies: Ischemia (especially inferior MI), Medications (CCB, Beta blockers etc.) Hyperkalemia, and ask about travel and send a Lyme titer if pertinent or you’re feeling fancy **Look closely at the EKG you’ll see pacemaker spikes (Red Arrows) which are followed by ventricular capture. The patient had a PPM which had not been check in > 10 years and battery failure. Thus the pacemaker was not firing**
0 Comments
What is the diagnosis?
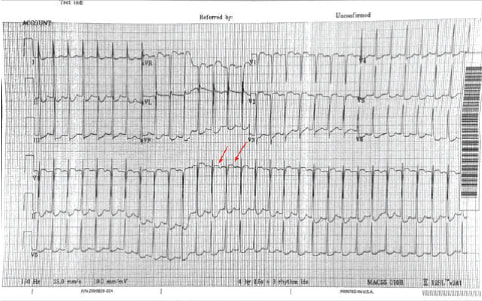
This is a narrow complex regular tachycardia. The differential diagnosis includes - sinus tachycardia, atrial flutter, paroxysmal supraventricular tachycardia PSVT which includes AVNRT - AV nodal reentrant tachycardia and AVRT (Atrioventricular Reciprocating Tachycardia), atrial tachycardia, irregular narrow complex tachycardias would include MAT (Multifocal Atrial Tachycardia) and Atrial Fibrillation. The most commonly seen etiology is PSVT. There do not appear to be P waves. However it is difficult to definitively rule out the other etiologies. One must always consider Atrial Flutter with 2:1 block when the HR is around 150. Best lead to see P wave activity is V1 (here red arrows show some blips which may be buried Ps) Is there a role for adenosine?
Adenosine will frequently terminate a PSVT and unmask underlying atrial flutter so can often be diagnostic Name an initial non-pharmacologic intervention
Vagal maneuvers. Consider using a 10 cc syringe and asking the patient to blow the plunger out ( Lin ALiEM 2012 ). Additionally there may be improved success with vagal maneuvers using postural modification as described in the REVERT Trial ( Wiki EM Summary ) Take Home Points
1. Always consider Atrial Flutter with 2:1 conduction if the HR is around 150s
2. Adenosine can be therapeutic (terminating PSVT) and and diagnostic (unmasking P waves) 3. Consider postural modification to vagal maneuvers Resources: Lin,Michelle (2012,June26) https://www.aliem.com/2012/06/tricks-of-trade-valsalva-maneuver-by/ Brady WJ, Laughrey TS, Ghaemmaghami CA. Cardiac Rhythm Disturbances. In: Tintinalli JE, Stapcyznski JS, Ma OJ, Yealy DM, Meckler CD, Cline DM, editors. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 8th ed. McGraw-Hill; 2011. Appelboam A. et al. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial. Lancet 2015 Oct 31;386(10005):1747-53 Inhaled toxins frequently cause asphyxiation and can be classified further as chemical asphyxiants, simple asphyxiants, and pulmonary irritants.
Chemical Asphyxiants include Hydrogen Sulfide and cyanide. Hydrogen sulfide typically presents with a sulfur-like smell, while cyanide is typically presented in the burning of plastics. Simple Asphyxiants are anything which replaces oxygen in the atmosphere, including carbon monoxide or dioxide, methane, helium, or nitrogen. These may be present in a mine or other industrial setting, and may classically present as an unconscious worker who was attempting to rescue another unconscious worker. Irritant gases cause pulmonary irritation from coughing to diffuse lung injury. Irritants are categorized by their solubility; highly soluble irritants typically have strong scents because they are easily mixed into the upper airway, while less soluble irritants are typically less rapid in onset and will result in lower airway complaints.
Current Definitions
Blood CulturesUtilization of blood cultures can assist the treatment of many patients, however not every patient requires blood cultures. Whenever drawn, you should obtain two sets of cultures (or 3 for endocarditis). A recent article found a number needed to treat was 250 for a change in treatment, however other studies have found blood cultures more useful. Major Criteria:
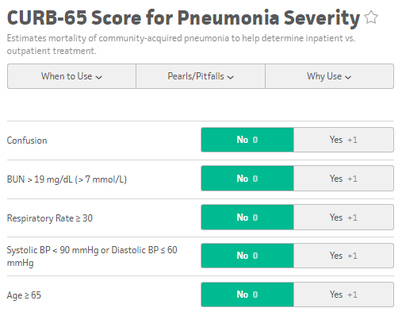
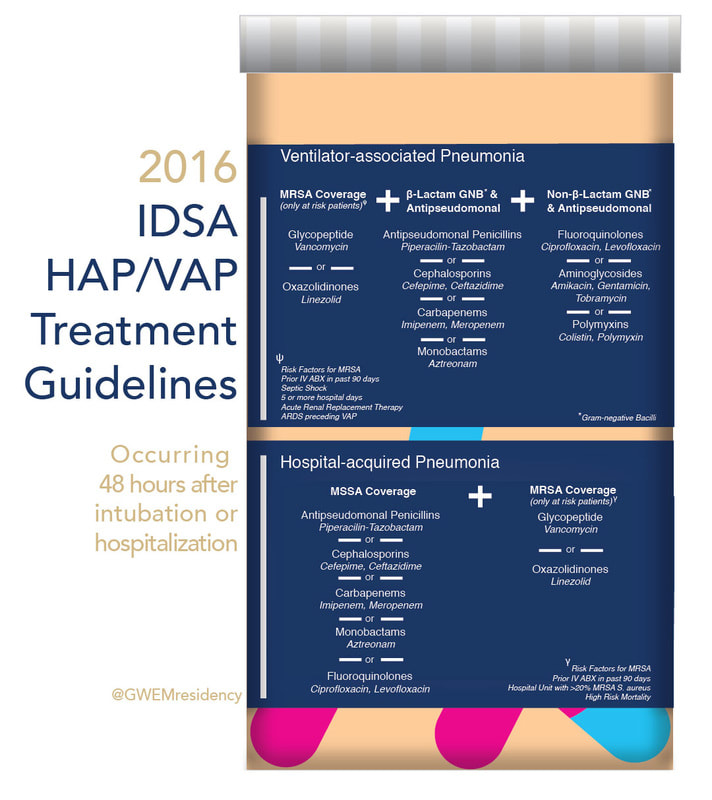
www.sciencedirect.com/science/article/pii/S0736467908004447?via%3DihubA blood culture is indicated by the rule if at least one major criterion or two minor criteria are present. Admission Criteria: CURB 65 and PSI/PORTPatients with CURB 65 scores 0-1 can potentially be discharged, however consider the patient's physical exam, oxygen saturation, and immunosupressed status, as the CURB 65 score does not take these into account. Those with a CURB 65 score greater than 3 should be considered for an ICU admission. The PSI/PORT score can also be used but is more thorough, including nursing home status, liver and heart disease status, as well as ABG data. While the CURB 65 has better specificity for identifying severe disease, the PSI/PORT score is more sensitive at identifying low-risk patients for discharge. TreatmentFor CAP, guidelines recommend Azithromycin or Doxycycline as azythromycin has increasing rates of resistance. In outpatients with co-morbidities or risk for resistance, you should consider levofloxacin or moxifloxacin. Patients admitted for CAP should be treated with single agent fluoroquinolone or dual agent treatment with ceftriaxone and azithromycin. ICU admitted CAP patients require an anti-pneumococcal betalactam (Ceftriaxone) and either azithromycin or fluoroquinolone. Treatment duration is typically 5 days.
45 M presents to the ED with lightheadedness after his LVAD “Low Flow” alarm sounded. He has a normal mental status, and MAP ~ 65 mmhg What is the rhythm?
Ventricular Fibrillation. There are no P waves nor organized QRS complexes. This distinction between coarse and fine V Fib is irrelevant. In theory fine V Fib indicates it has been a longer duration but management is not different. You may look at the EKG and question whether the patient has Torsades. The initial distinction is irrelevant as the patient is likely unstable / pulseless and needs electricity. Torsades can only be diagnosed with prolonged QT on the patient’s preceding or ensuing EKG. How would you typically manage this rhythm?
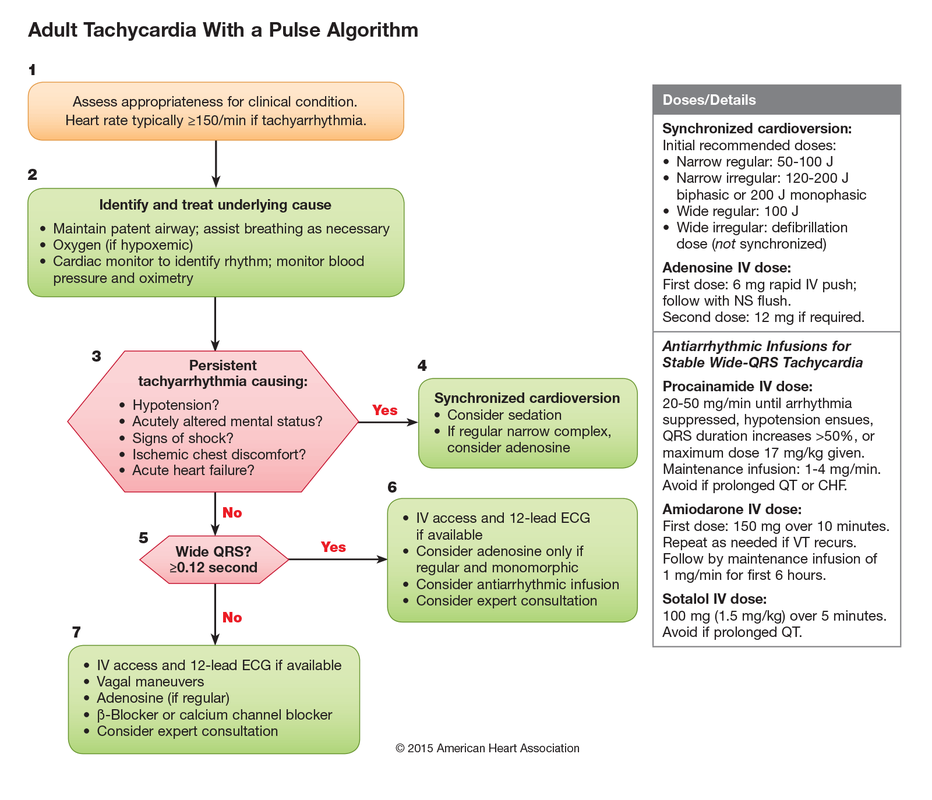
ACLS approach to tachycardias:
1.Does the patient have a pulse? 2. Shockable rhythm or not? If Pulse and unstable → Synchronized cardioversion (the electricity is timed to the cardiac cycle). If the patient is pulseless then analyze the rhythm and determine is it “Shockable” (Pulseless VTach or VFib) or “Non-shockable” (PEA or Asystole). The first step is immediate CPR in both scenarios until you can get the defibrillator to defibrillate the shockable rhythms (electricity not timed to cardiac cycle). ****THESE ARE THE PATIENTS THAT ACLS SAVES**** How would you manage this rhythm in lvad patients?
Call for help when they hit the door. You should NOT perform CPR in an LVAD patient unless you can confirm they are in cardiac arrest. Most often the pump needs troubleshooting. Arrhythmias are not uncommon. You can attempt chemical cardioversion (amiodarone) or electrical cardioversion. Pads do NOT go over the LVAD. Use the anterior/posterior positions.
Take Home Points 1. It is not important to distinguish between types of VFib → the answer is defibrillation 2. Torsades de Pointes can only be diagnosed if the preceding/ensuing EKG has prolonged QT 3. Do NOT perform CPR on LVADs unless Cardiac Arrest confirmed (eg MAP 0 mmHg) 4. When performing defibrillation or cardioversion in LVAD patients place pads Anterior / Posterior Resources: Partyka C and Taylor B. Review article: ventricular assist devices in the emergency department. Emerg Med Australas. 2014 Apr; 26(2): 104-12. Link MS, Berkow LC, Kudenchuk PJ et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015; 132:S444 Massive Pulmonary Embolism
Submassive Pulmonary Embolism
ManagementIn patients with severe hypoxia and shortness of breath, consider NIPPV early, even before CT diagnosis. As the patient has increased Right sided failure and RV dilation, the patient will continue to have worsening RV ischemia and decreased RV contractility. As RV afterload increases you begin having worsening right sided failure and worsening cardiac output. In patients who require inotropes, consider norepi and dobutamine.
Systemic ThrombolyticsThe use of systemic thrombolytics are supported by most protocols. Many RTCs have evaluated the use of thrombolytics, including half-dose and catheter-directed TPA. While mortality improves with thromolytic use in massive PEs, RTCs evaluating lytics in submassive PEs have been mixed. Catheter-directed intervention is a safe and effective treatment for both submassive and massive PEs.
|
Categories
Archive
February 2018
Please read our Terms of Use.
|