|
For treating Candida Vaginitis in early pregnancy, ACOG recommends local treatment instead of oral diflucan. This is based on studies that show higher doses (400-800 mg) of oral diflucan has been linked to birth defects. Although a 2013 NEJM cohort study found no association between diflucan and birth defects.
When treating pregnancy women for a UTI in early pregnancy, Nitrofurantoin or Bactrim are both not recommended as a first line agent. A Case-Control study published in 2009 showed an association between treatment with these medications in first trimester and malformations. While there are several limitations to this study, ACOG recommends avoiding these two medications in the first trimester. During the 2nd and 3rd trimester, sulfonamides and nitrofurantoin may be used as first-line therapy. Prescribing these in the first trimester is still considered appropriate when no other alternative is available. Penicillins, erythromycin, and cephalosporins have not been found to have any associations with birth defects.
0 Comments
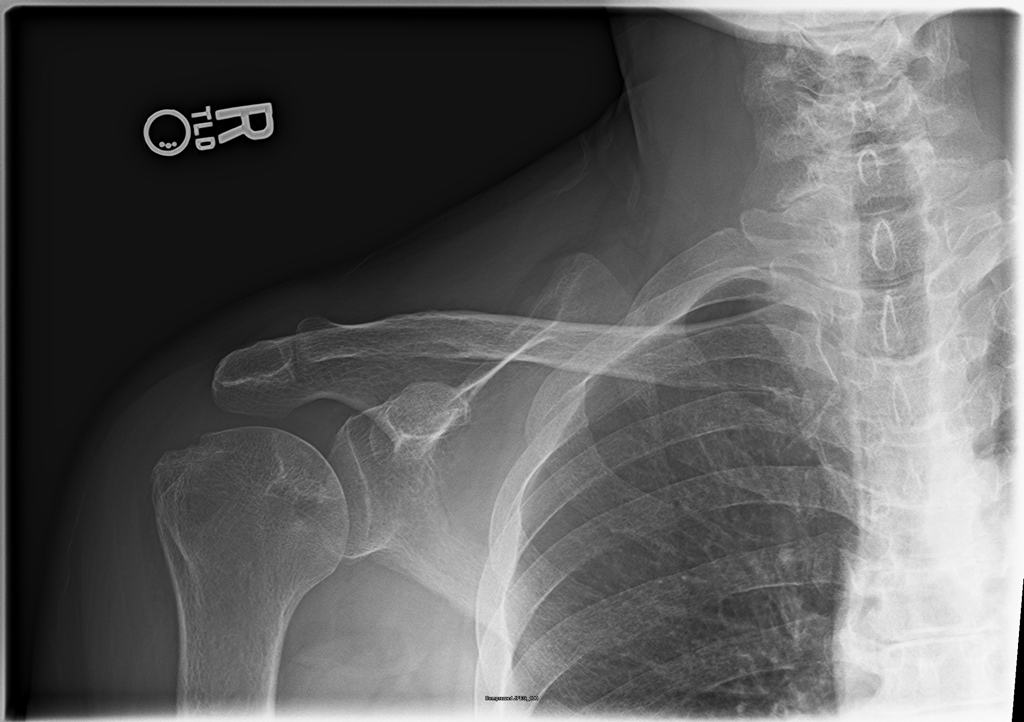
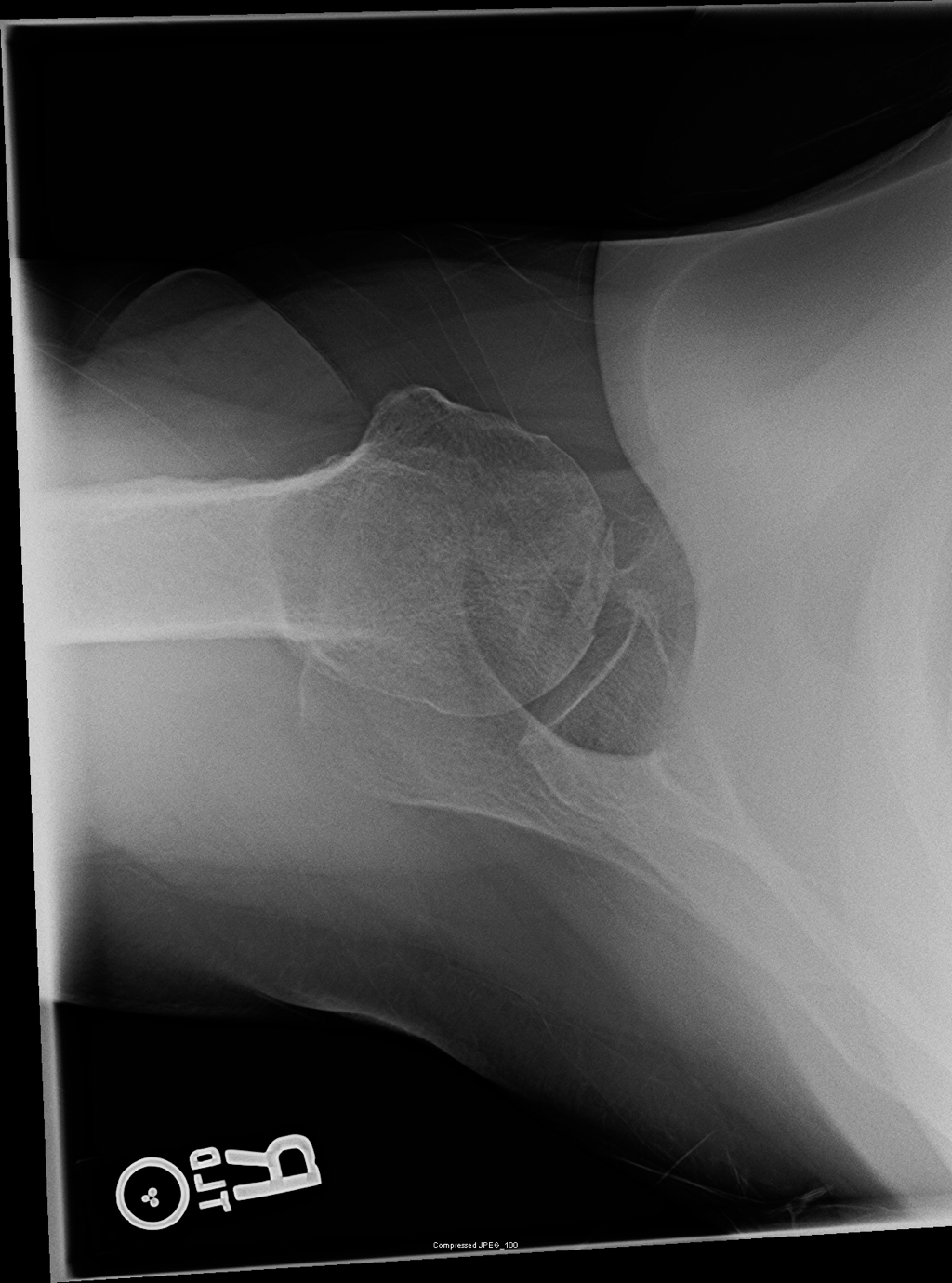
57 yo female with a history of hypertension, osteoarthritis, and asthma with chronic steroid use, presenting with multiple complaints, including chronic right shoulder pain that has been worsening the past week. The pain is constant and worse with any ROM of the right shoulder. Physical exam, including Spurling's Test, is otherwise unremarkable. On further discussion, the patient has had a remote hip replacement for avascular necrosis, and no recent traumas.
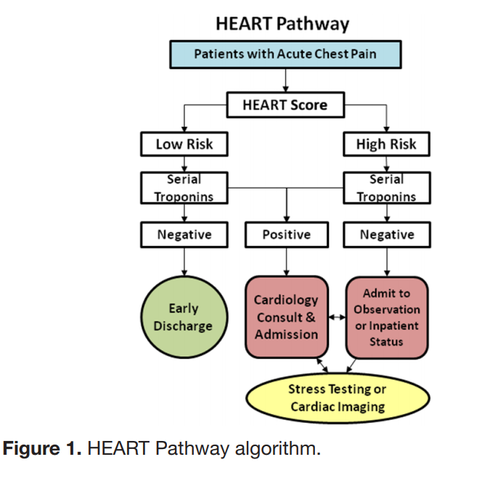
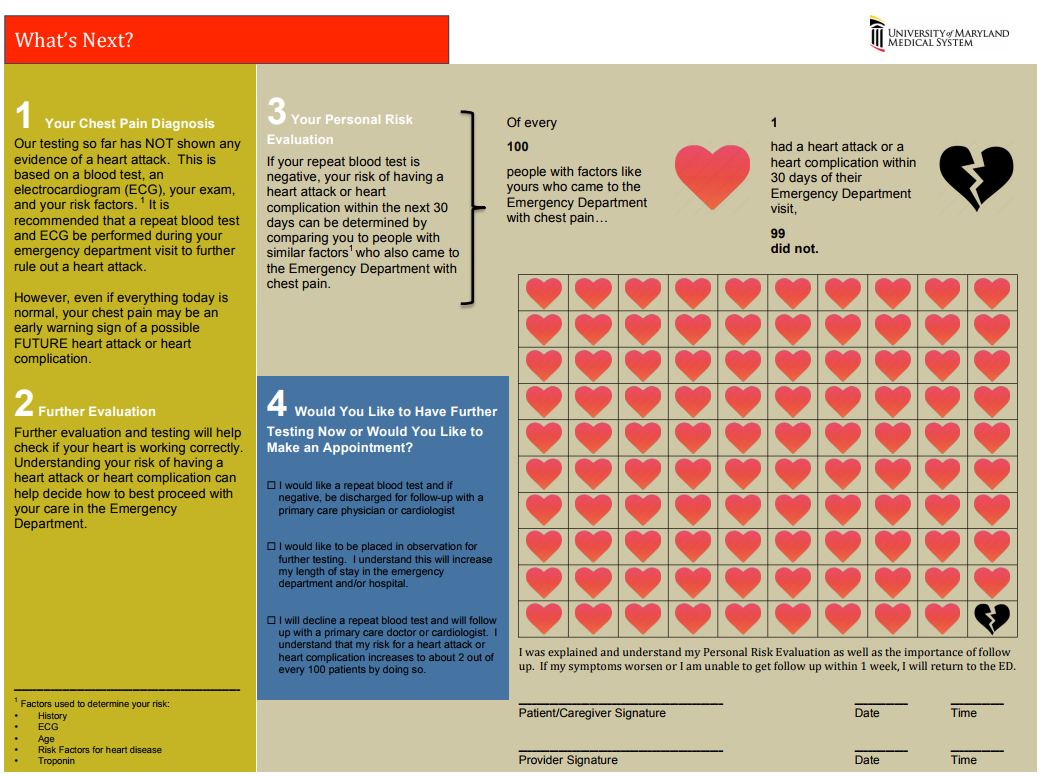
The “Delta Trop” is not a rule out test! It should be used in conjunction with the HEART score to have a conversation with the patient about risks/benefits of discharge vs admission during a low-risk chest pain evaluation. The “Delta Trop” refers to serial troponin testing, anywhere from 2 to 6 hours between the first and second troponin. As troponin testing has improved, the time between each test has been lowered. The most recent data recommends 3 hours between each troponin when the high-sensitivity test is used. The delta troponin is not a “Rule Out”; it is used in addition to the rest of the patient’s visit to help risk stratify them into low, moderate, or high risk chest pain. The HEART Pathway combines the patient’s HEART score with two serial troponins at zero and three hours. Observational studies showed 20% of patients with chest pain can be safely discharged utilizing this protocol, while maintaining a negative predictive value of Major Cardiac Event at >99%. This is actually a lower rate of MACE than the traditional HEART score alone (1.0% versus 1.7%). A recent controlled trial increased early discharges by 21.3%, decreased cardiac testing by 12.1%, and decreased length of stay by 12 hours! Just because we are discharging people, however, doesn’t mean they have been ‘ruled out’ for cardiac issues. Remember, 1% of those discharged had a major cardiac event within 30 days. The “Delta Trop” should be used as a shared decision making tool where the patient is provided the information and risks/benefits of admission versus discharge. Attached is the University of Maryland shared decision making tool, which is used in conjunction with a bedside discussion, to explain the risks and benefits.
Shared Decision MakingWhen you identify a patient with a low heart score (1-3) you can use this dotphrase to improve your documentation of your shared decision making conversation, and to make sure you are not forgetting alternative causes of chest pain. Remember, that by hitting “F3” your cursor will jump to the next “_” Patient HEART score 0-3, with risk of MACE 1.7% within 6 weeks, discussed with patient the potential for symptoms to be cardiac in nature and the need for follow up and return precautions. Other potential causes of the patient's presentation were considered; PERC _. Well's _. Pain not consistent with aortic etiology. Physical exam reassuring without signs of pneumothorax, pulmonary infection, heart failure exacerbation, or respiratory failure. Initial troponin negative. Discussed with patient the possibility of approximately 2% of an adverse cardiac event within the next 4-6 weeks, as well as options for further treatment, including observation admission, a second troponin at 3 hours, or discharge. After this discussion, the patient elected to _.
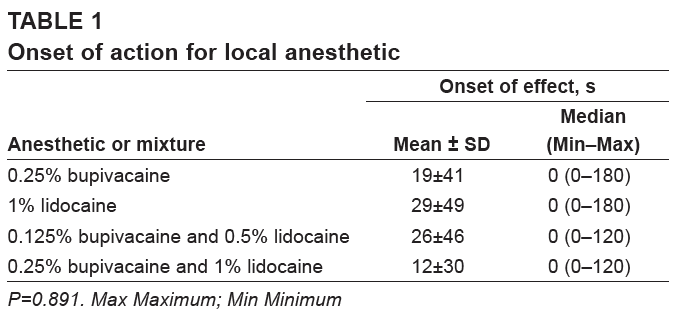
Bupivacaine and lidocaine are often used concurrently, in theory, to combine the more rapid onset of lidocaine and the longer duration of bupivacaine. However, multiple studies, including a 1996 Journal of Podiatric Medicine article and a 2013 Canadian Journal of Plastic Surgery study have found no statistical difference between the anesthetics with regard to onset of action.
Lithium is an effective treatment for bipolar disorder, and is known to decrease rates of suicide associated with affective disorders. Additionally, lithium is uncommonly used to augment treatments for depression, aggression, and PTSD. Unfortunately, lithium is also frequently the cause of toxic ingestions due to its narrow therapeudic window, renal clearance, and utilization for intentional overdoses.
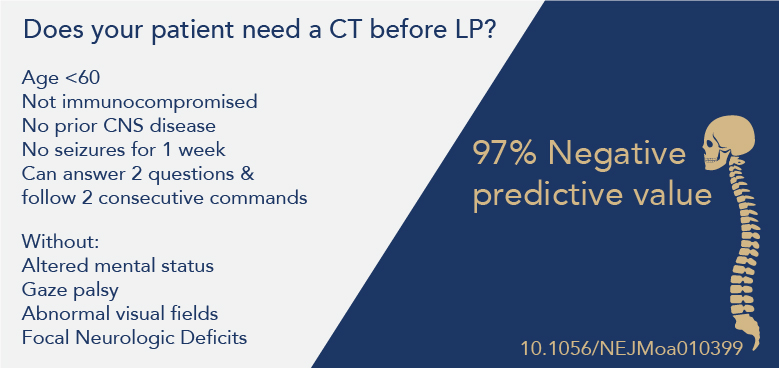
Before every lumbar puncture many providers reactively get a CT to rule out a mass or reduce the risk of herniation, However, not every patient requires a CT.
Diagnosing and treating undifferentiated shortness of breath is usually an easy task, but sometimes the etiology can be difficult to determine. Other times, there may be multiple causes. Here are a list of "C's" to keep in mind in patients with shortness of breath.
Neonates (<28 days of age) are a fragile population that can present in life-threatening distress that requires immediate evaluation and treatment. As such, utilizing a systematic approach can help identify and treat the most common causes of neonatal distress. As more hospital nurseries discharge patients earlier, emergency departments must be ready to evaluate, diagnose, and treat neonatal emergencies. For more information; ACEP "The Misfits" The MisfitsThe Misfits is a useful mnemonic for neurologic changes in the neonate, and can be expanded to neonatal distress in general to aid in a systematic approach to all neonates in distress. Keep in mind that neurologic changes in the very young may be subtle and difficult to diagnose.
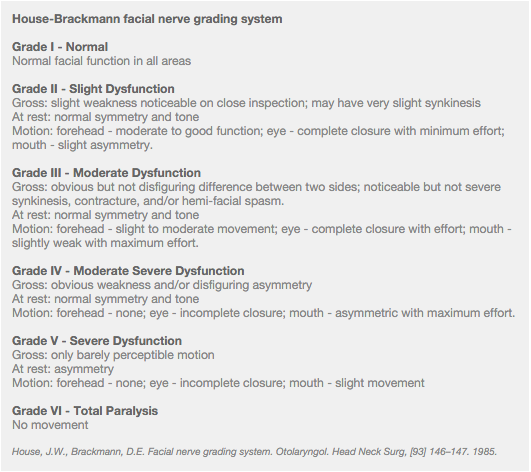
Intestinal EmergenciesTeaching Pearl: Bell's Palsy can be easily diagnosed by clinical examination, however the treatment varies depending on severity and the patient's own medical history. You should never prescribe steroids longer than antivirals, due to the possibility of a viral infection progressing while steroids are continued. Additionally, any patient who has a House-Brackmann score of IV or more, must go home with instructions and material to tape their eye shut at night, otherwise, they risk corneal abrasions and ulcers. You should also consider antivirals, and be sure to check their auditory canals for signs of herpetic skin lesions.
|
Categories
Archive
February 2018
Please read our Terms of Use.
|
||||||||||||||||||