|
Lithium is an effective treatment for bipolar disorder, and is known to decrease rates of suicide associated with affective disorders. Additionally, lithium is uncommonly used to augment treatments for depression, aggression, and PTSD. Unfortunately, lithium is also frequently the cause of toxic ingestions due to its narrow therapeudic window, renal clearance, and utilization for intentional overdoses. Lithium ToxicityToxicity can be either acute or chronic. Chronic lithium users usually experience at least one episode of toxicity while under treatment. This is due to its narrow therapeudic window of 0.6-1.2 mEq/L. Decreases in GFR or dehydration is the most common cause of chronic toxicity, followed by increased dosing of lithium. Chronic toxicity may present with mild symptoms of toxicity, such as increased tremor, slurred sppech, and mild lethargy.
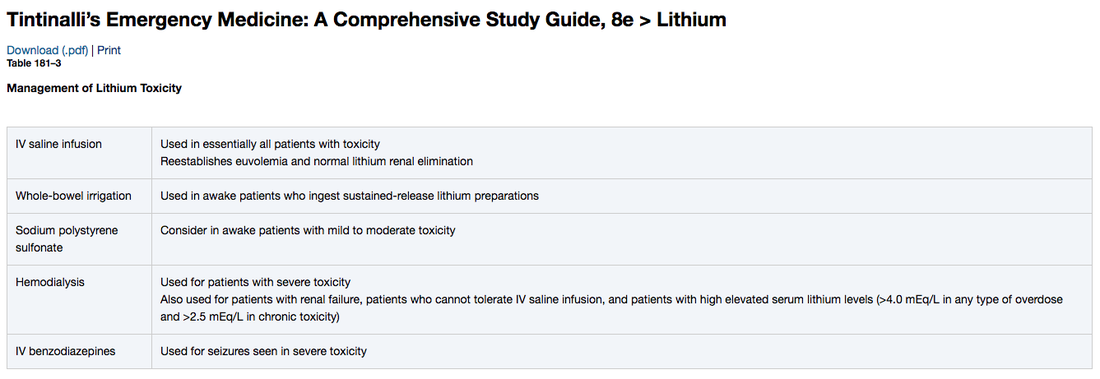
TreatmentAfter stabilization and evaluation for co-intoxications, treatment for lithium toxicity is to hydrate with a combination of IV fluids. Initially, normal saline should be used as most patients will have a sodium and volume deficit. Diuretics, especially loop and thiazide diuretics should not be used, as they can promote water loss and lithium retention. Whole-bowel irrigation is useful in those who have ingested sustained release versions of lithium, but is not indicated in the ingestion of immediate-release tablets. Early adjustments of saline therapy and the addition of free water can prevent hypernatremia in patients with DI. Kayexalate has been down to reduce lithium concentrations, however be cautious if your patient is an aspiration risk. Once serum lithium levels are known, dialysis may be required to treat severe toxicity, when serum lithium concentration is greater than 5 mEq/L, or greater than 4 mEq/L in patients with renal impairment. Additionally, despite lithium levels, patients with decreased level of consciousness, seizure, or life-threatening complications are canditates for dialysis. Nephrogenic Diabetes InsipidusNephrogenic DI occurs when the kidneys are unable to concentrate urine, causing hypotonic urine leading to hypernatremia and free water loss. This is secondary to lithium interfering with reupkate of water and failure of the kidney to produce concentrated urine. If you really want to know, lithium dereased the number of aquaporin receptors in the membrane. Although not all patients will present with hypernatremia, you should get repeat BMPs during resuscitation to help identify and correct any sodium abnormalities. Thyroid FunctionLithium inhibits release of thyroid horomone, leading to hypothyroid and goiter, both in chronic users and toxicity. Long term, lithium can also increase thyroid autoimmunity and induce hyperthryoidism (Graves Disease). EKG ChangesAlthough rare, patients have have flat t waves anf prolonged Qtc.
0 Comments
Leave a Reply. |
Categories
Archive
February 2018
Please read our Terms of Use.
|