|
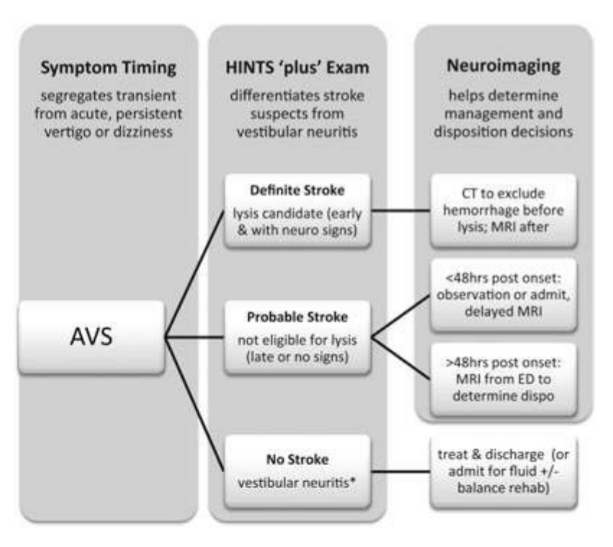
Dizziness can be difficult to assess in the ED given the vast range of etiologies and varying ways patients interpret their symptoms. Additionally, not all patients with emergency conditions will present with obvious focal deficits. A clinical decision making rule (HINTS) can help to more rapidly identify stroke patients to initiate acute therapies faster. The HINTS rule outperforms ABCD2 for stroke diagnosis in the ED when performed by qualified practitioners in patients with Acute Vestibular Syndrome. Typically, patients with peripheral vertigo appear to have an acute change and may be very ill appearing, with nausea and vomiting and severe vertigo symptoms. Those with central vertigo typically have a more insidious onset, constant symptoms, and typically less severe symptoms. Common Causes
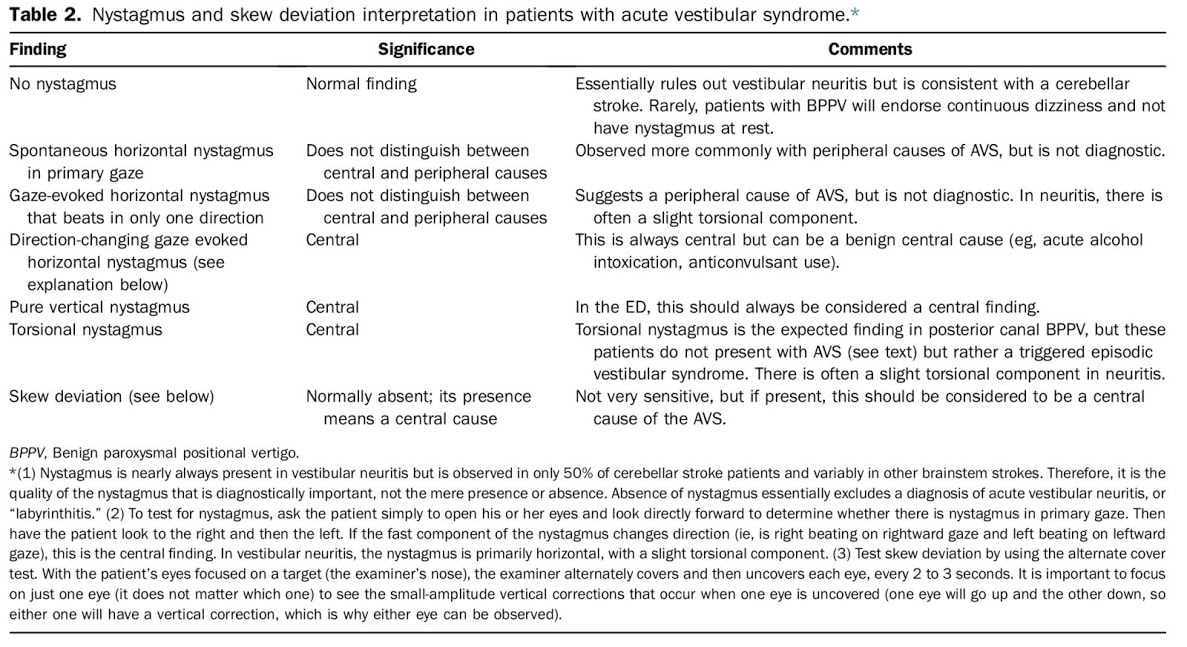
Signs of a Central CauseSymptoms of a central vertigo may be difficult to identify. Typically, there are some of the "5 D's"
HINTS ExamLINK TO 8 MINUTE HOW TO VIDEO Indications of a Central Cause:
Pharmacologic Management
0 Comments
Auricular Hematoma
Otitis ExternaOtitis externa is frequently caused both by swimmer and water exposure as well as the use of household items to 'clean out' the ear. This should be treated with cipro otic drops, and patients should not be placed on oral antibiotics as this will only increase the risk for fungal infection and not assist in treating the bacterial infection. Consider placing an ear wick to help increase the amount of antibiotic which reaches the infected area. Bullous MyringitisAn infection of the ear drum that causes severe pain and loss of hearing. On examination a red or clear blister will be present on the ear drum. Treatment is antibiotics and rupturing the blister. Tympanic Membrane PerforationsTypically due to blunt trauma or direct penetrating trauma from Q-tips or other objects. Ciprodex antibiotic drops, and water precautions should be given, as well as ENT followup. Those with severe symptoms such as hearing loss, vertigo, or nystagmus should have urgent ENT followup. Otitis MediaOver 70% of OM is viral, but it is difficult to determine viral vs bacterial. Most bacterial infections are strep pneumo (50%). On exam the patient will have bulging of the TM or an air-fluid level. To accurately diagnose OM, you should be unable to move the TM with suction. Treatment is to either wait and watch or provide high-dose amoxicillin. Sudden Sensorineural Hearing LossAcute loss of hearing without an external or conductive cause. It is sudden (<72 hours) and unilateral, caused by viral, ischemic, or auto-immune causes. Syphilis and idiopathic intracranial hypertension can both cause acute unilateral hearing loss. Many cases are idiopathic. Treatment is either PO steroids or direct steroids to the middle ear, and urgent ENT followup. Antivirals should only be given if there are signs of a vesicular lesion. Bell's PalsyPatients presenting with symptoms of Bells Palsy should have a full history and physical examination to identify facial paralysis and possible causes, including evaluated for lesions of the TM concerning for Ramsay Hunt Syndrome. The AAO do not recommend routine lab testing or imaging in patients with Bell's Palsy, unless the patient lives in an area with endemic Lyme Disease. Patients should be treated with both oral antiviral AND oral steroid treatment together within 72 hours of symptom onset. Antiviral treatment alone is not recommended, however steroids alone may still have benefit. Patients should be sent home with eye protection and eye drops to prevent trauma and corneal abrasions or ulcers. AAO Guidelines.
CPR induced consciousness is characterized by a patient waking up, moving their limbs, or even fighting responders during compressions. Typically, when the providers stop compressions, either for a pulse check or because of assumed ROSC, the patient stops moving and again goes unresponsive. This has been described in both pre-hospital and hospital settings, and with improvement of CPR quality, will occur more frequently. What is CPR-Induced Consciousness?CPR Induced Consciousness occurs when CPR generates sufficient cerebral perfusion pressure (CPP) to allow for consciousness. CPP correlates closely with brain oxygenation. In 1995, the topic was first asked if patients should be sedated during CPR, but this was based off the idea that they patient may be conscious during the peri-arrest episode, not during the actual resuscitation itself. In a prospective study of 2060 victims of cardiac arrest, 46% of survivors reported memories of the CPR. Single images were placed on shelves visible to the patient to assess visual awareness during resuscitation, and all survivors were interviewed in a two step interview process. Most patients recalled themes of fear, bright light, violence or a sensation of being persecuted, seeing family, or recalling events that occured after ROSC. 2% actually recalled seeing and hearing actual events related to their resuscitation, including one episode that was verifiably accurate. (AWARE, S. Parnia et al. / Resuscitation 85 (2014) 1799–1805) A systematic review of case reports and published articles in 2015 found only 10 cases of actual awareness, excluding all near-death experiences, animal models, and non-purposeful movements. In 5 of 10 cases, CPR was initiated immediately and occured in-hospital. In all out-of-hospital cases, CPR began within 1-minute. All patients in the review had purposeful arm movements, while there was also a range of other findings including eye opening, localizing to painful stimuli, and even verbal communication, including adhering to instructions being given. A retrospective review of data from Victoria, Australia in 2017 found that CPR-Induced Consciousness is reported in approximately 0.7% of out-of-hospital cases, and increased over time from 2008 to 2014, presumptively from improvements in CPR quality. 87% of patients had body movement, 29% had vocalizations, and 20% had eye opening. Management of CPR Induced Consciousness: Due to higher-quality CPR, an unintended consequence has been CPR-induced consciousness, leading to some EMS agencies to creating protocols for sedation during CPR. These include IV or IM Ketamine (0.5-2mg) as well as midazolam. (Rice, 2016).
There is data showing that treating CPRIC is not associated with worsening outcomes or increased mortality, so you should consider treating CPRIC with either a small, repeated benzodiazapine or ketamine boluses. For treating Candida Vaginitis in early pregnancy, ACOG recommends local treatment instead of oral diflucan. This is based on studies that show higher doses (400-800 mg) of oral diflucan has been linked to birth defects. Although a 2013 NEJM cohort study found no association between diflucan and birth defects.
When treating pregnancy women for a UTI in early pregnancy, Nitrofurantoin or Bactrim are both not recommended as a first line agent. A Case-Control study published in 2009 showed an association between treatment with these medications in first trimester and malformations. While there are several limitations to this study, ACOG recommends avoiding these two medications in the first trimester. During the 2nd and 3rd trimester, sulfonamides and nitrofurantoin may be used as first-line therapy. Prescribing these in the first trimester is still considered appropriate when no other alternative is available. Penicillins, erythromycin, and cephalosporins have not been found to have any associations with birth defects. What is the differential diagnosis?
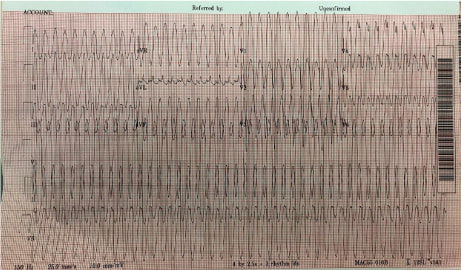
When approaching an EKG with tachycardia, one should first determine: is the QRS complex wide or narrow? And is the rhythm is regular or irregular? This patient’s EKG is regular with a wide QRS complex. Differential Diagnosis - Ventricular Tachycardia, SVT with Aberrancy (Bundle Branch Block or accessory pathway) or paced rhythm. No pacer spikes are seen which leaves VT and SVT with Aberrancy. A number of decision aid tools exist to assist in distinguishing (Brugada is most common) but are cumbersome. What's the final diagnosis?
Wide complex tachycardia likely Idiopathic Monomorphic VT originating from the RVOT. VT = QRS complexes originating in ventricle and > 30 second duration. < 30 second = NSVT. VT is classified as monomorphic (no beat to beat variation in QRS complex morphology) and polymorphic. VT can have ischemic or idiopathic etiologies. This 19 yo was unlikely to have ischemic heart disease. Management?
General Rule - Treat wide complex tachycardias as VT and cardioversion is always the safest option. Per ACLS STABLE patient with wide complex tachycardia that is REGULAR → an adenosine challenge can be attempted. This will terminate SVT and some Idiopathic VTs (eg RVOT). If unsuccessful ⇒ Procainamide Take home points:
1. Differing VT from SVT with aberrancy is not essential. It is always safest to treat as VT.
2. An adenosine challenge may be attempted for WCT only if the following two conditions are met: The patient is STABLE & The rhythm is REGULAR Sources: Link MS, Berkow LC, Kudenchuk PJ et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015; 132:S444 |
Categories
Archive
February 2018
Please read our Terms of Use.
|
||||||||