- by Brian D'Cruz DC has highest prevalence of HIV in country: 2.5%
How to recognize HIV pateitn at Fairfax
HIV Types
0 Comments
 by Stas ARDS
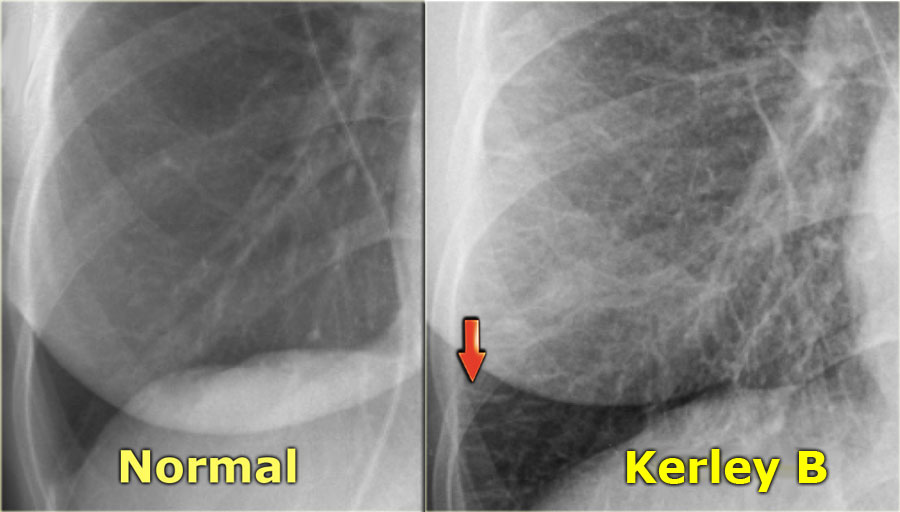
Cardiogenic (interstitial) edema
Case
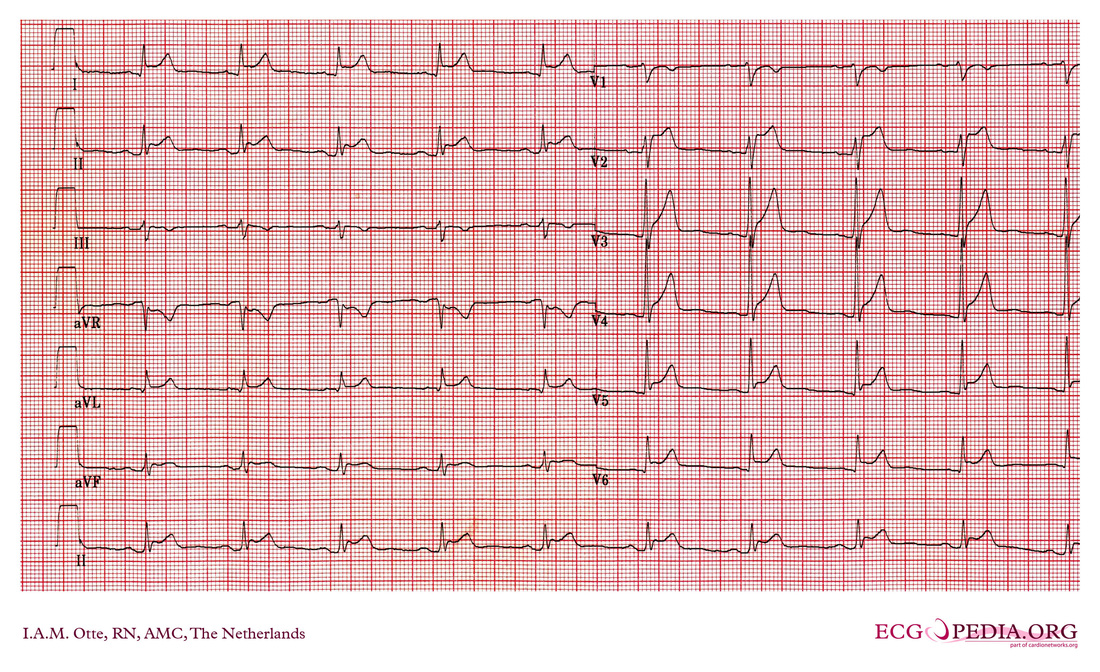
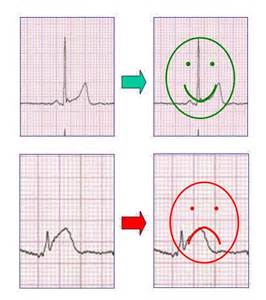
CC: 39M c/o right hip pain VS: WNL ...waiting 6 hours ot be seen HPI: dull, constant aching x 3 months, worse iwth physical activity, acutely worse after basketball today, happening more often No trauma (remote surgery of right knee), has unprotected intercourse with monogamous partner Soc/Fam: remote drug history (not IV); active, fit, plays basketball frequently ROS: sporatic back pain, infrequent night sweats over summer, occasional numbness/tingling in right foot PE: right hip pain with add/ab, prominent thoracic spine DDx: traumatic injury/repetititve injury, cauda equina, epidural hematoma, joint infection, ankylosing spondylitis, bony fracture, discitis Labs: normal XR hip: erosion at hte femoral head-neck junction, osteopenia, loss of joint space Inflammation of the pericardium, usually after a viral infection, presenting classically with chest pain that improves when leaning forward, tachycardia, and dyspnea. Can be associated with a friction rub or pericardial effusion. In pericarditis four stages can be distinguished on the ECG:
Sources:
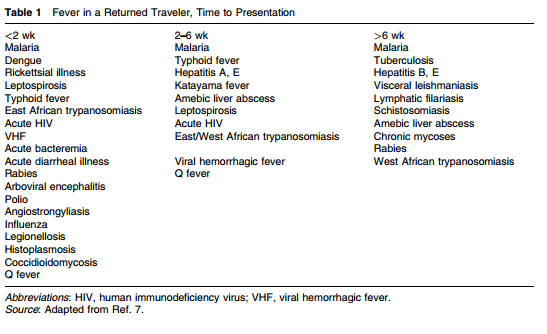
ECGpedia; http://en.ecgpedia.org/index.php?title=Pericarditis Your differential diagnosis for a traveler who presents with an illness should include not only the common causes you see everyday, but also more rare diseases they could have been exposed to during their travels. Keep in mind that the exact etiology may not be identified. Make an accurate travel timeline, and calculate the incubation period for the patient, and avoid artificially narrowing your focus to just tropical diseases. Ask about prophylaxis, immune status, and any higher risk travel history including local food, sexual interactions, and where they stayed during the trip. The CDC has a great site to help identify people at risk for certain diseases depending on their travel. When concerned, get an infectious disease consult early in the evaluation, and consider admission in patients who have a negative initial thick/thin smear. MalariaMalaria is caused by four different plasmodium parasites, with Plasmodium falciparum being the most predominant cause of mortality. The majority of patients present within four weeks of their return, and 60% are hospitalized with complications including cerebral malaria. Risk factors for severe disease and potential mortality include not taking chemoprophylaxis and a delay in diagnosis. There are no pathognomonic historical or physical exam findings, and malaria cannot be ruled out without lab testing. Classically, malaria presents with cyclical fever, chills, and sweats. The pattern of fever may not be readily apparent, and can be associated with anemia, thrombocytopenia, and CNS dysfunction. Diarrhea or other symptoms should not deter you from testing. Thick and Thin smears are used to diagnose malaria. Thick smears provide a higher sensitivity, while the thin smear is used to speciate the parasite. The CDC recommends three sets of blood smears to ensure high enough sensitivity to properly diagnose all patients, and higher fevers are not always associated with a higher parasite load. The only drug currently licensed in the US is Quinidine, although Artemesinins is currently undergoing trials with the CDC. Quinidine should be used in combination with a second schizonticide, such as doxycycline, tetracycline, or clindamycin. Prior to starting Quinidine evaluate for QRS widening or QTc prolongation as Quinidine can cause widening and prolongation. Source:
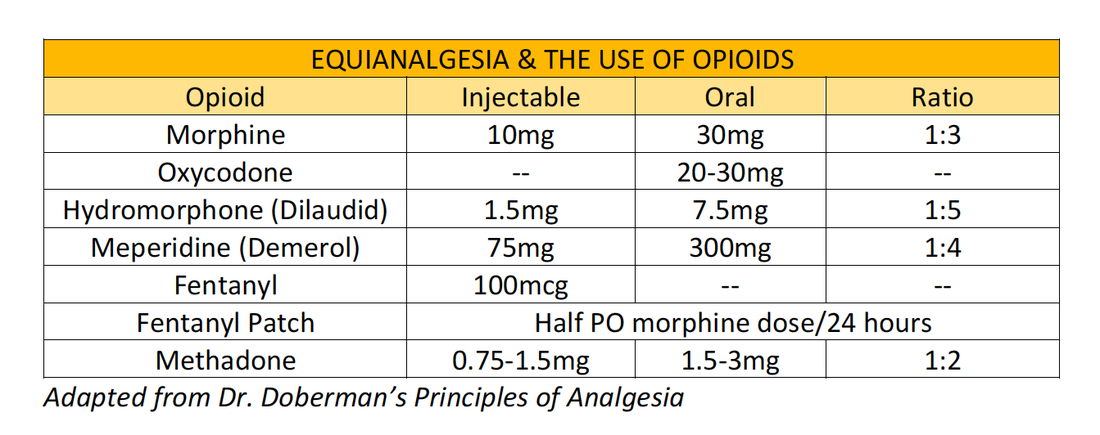
Infectious diseases in critical care medicine (1-4200-9240-5, 978-1-4200-9240-0), 3rd ed. / Cunha, Burke A. Informa Healthcare USA, 2010 Adapted from Dr. Doberman's Principles of Analgesia, Palliative & Geriatrics Make sure you are appropriately treating your patient's pain!
Use the appropriate dosages at the appropriate intervals; PO medications should be redosed every 3-4 hours for short-acting medications. IV opioids should be redosed every 1-2 hours. Titrate your dosing to patient comfort. In severe pain, titrate rapidly with short acting opioids, and change to longer acting medications when pain relief is achieved. During in-patient services, always remember to provide a breath through pain medication that provides 10-20% of their normal 24 hour oral dose, or 50-100% of their hourly IV rate. |
Categories
Archive
February 2018
Please read our Terms of Use.
|