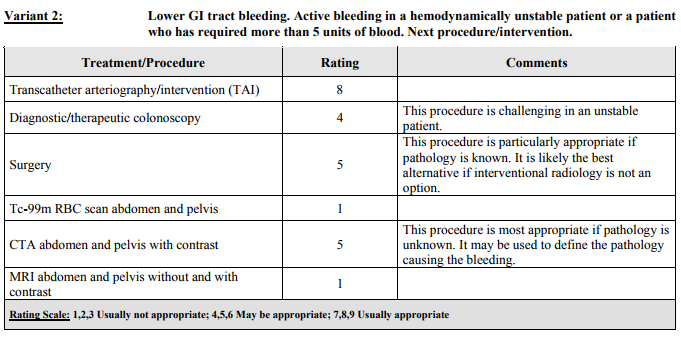
Causes of Lower GI BleedingColorectal sources, such as hemorrhoids, are the most common causes of LGIB in all age groups, followed by diverticular disease, colitis, polyps, and maligancies. Diverticular bleeding from an eroded artery is painless and can be brisk, but typically is self resolving, but frequently recur. Right-sided diverticulosis is more likely to bleed, although left-sided diverticulosis is more common. A concomitant diverticulitis is exceptionally rare with a bleeding diverticula. Vascular causes, such as an AV malformation or angiodysplasia can occur in the small or large bowel, and typically associated with a chronic process and increases with aging. These are less commonly occurring. Meckel's diverticulum contain ectopic gastric tissue, which can secrete gastric enzymes, eroding the mucosal wall and causing bleeding. Meckel's is rare, but can be an important cause of LGI bleeding in younger patients. There are numerous other causes for LGI bleeding, including infectious colitis, inflammatory bowel disease, trauma, or anticoagulation use. Determining the SourceHematochezia is bright red or maroon-colored rectal bleeding, which indicates either a brisk UGI or a lower GI bleed. Hematemesis and hemodynamic instability should accompany a brisk UGI bleed. Melena is dark or black-colored stools which typically represents an UGI bleed, but could represent a LGI source. ImagingACR recommends CTA in those patients who have an unknown source of LGI bleeding, and may be used to define the pathology causing the bleeding. The tagged RBC scan has fallen out of use in unstable patients with an ACR rating of 1. DispositionHigh-risk populations include:
Low-risk population include;
Currently, there is no reliable scoring system to risk stratify patients with LGI bleeding. Patients may be candidates for discharge with followup are those who have a mild LGI bleed with an obvious source (such as hemorrhoids), who have no bright red blood or maroon/melanotic stool on examination, and are hemodynamically stable without major comorbidities.
0 Comments
Leave a Reply. |
Categories
Archive
February 2018
Please read our Terms of Use.
|