|
In the US, approximately 200,000 people are diagnosed with a new or recurrent pulmonary embolism each year. More than twice this many are diagnosed with a DVT without PE, and 1 in 300 ER patients are diagnosed with a DVT. The lifetime risk of a DVT is 2-5%, and the incidence of DVT increases with age. DVTs can lead to a pulmonary embolism, which is one of the leading causes of sudden, nontraumatic death in the US. Most DVTs are unprovoked, with an increased risk for reoccurrence, requiring a longer treatment period than those with provoked DVTs from drugs, trauma, or surgery. Typically, DVTs begin at the valves of the veins. Proximal DVT include Femoropopliteal (FP) ilieofemoral (IF) DVTs, and account for 80% of symptomatic DVTs. Distal DVTs of the calf account for only 20% of symptomatic DVTs.
0 Comments
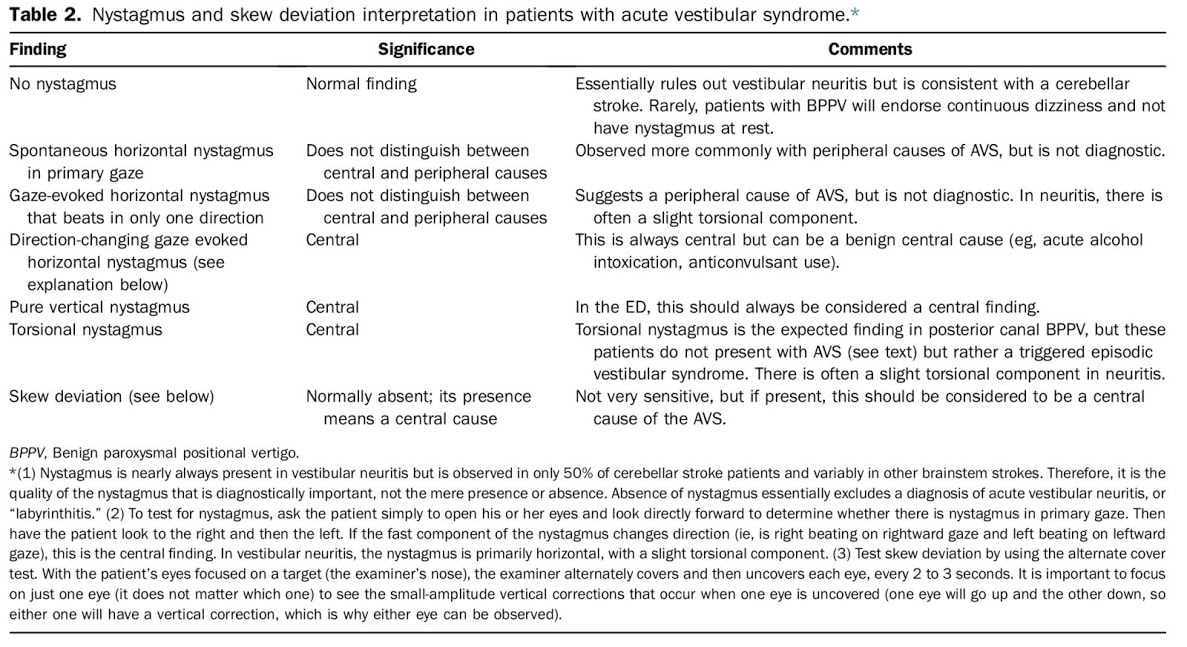
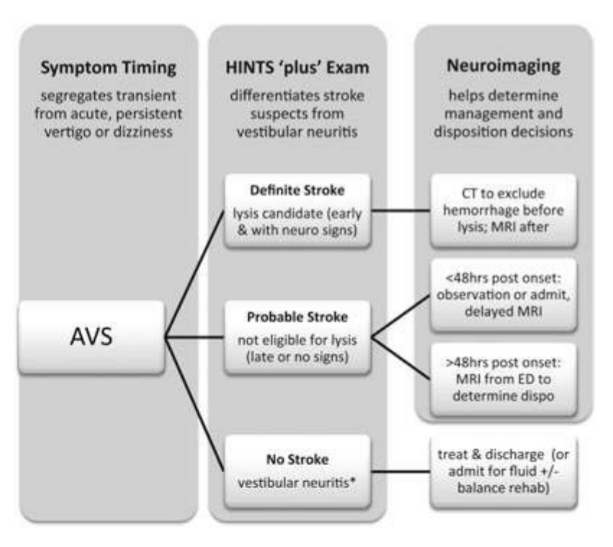
Dizziness can be difficult to assess in the ED given the vast range of etiologies and varying ways patients interpret their symptoms. Additionally, not all patients with emergency conditions will present with obvious focal deficits. A clinical decision making rule (HINTS) can help to more rapidly identify stroke patients to initiate acute therapies faster. The HINTS rule outperforms ABCD2 for stroke diagnosis in the ED when performed by qualified practitioners in patients with Acute Vestibular Syndrome. Typically, patients with peripheral vertigo appear to have an acute change and may be very ill appearing, with nausea and vomiting and severe vertigo symptoms. Those with central vertigo typically have a more insidious onset, constant symptoms, and typically less severe symptoms. Common Causes
Signs of a Central CauseSymptoms of a central vertigo may be difficult to identify. Typically, there are some of the "5 D's"
HINTS ExamLINK TO 8 MINUTE HOW TO VIDEO Indications of a Central Cause:
Pharmacologic Management
Auricular Hematoma
Otitis ExternaOtitis externa is frequently caused both by swimmer and water exposure as well as the use of household items to 'clean out' the ear. This should be treated with cipro otic drops, and patients should not be placed on oral antibiotics as this will only increase the risk for fungal infection and not assist in treating the bacterial infection. Consider placing an ear wick to help increase the amount of antibiotic which reaches the infected area. Bullous MyringitisAn infection of the ear drum that causes severe pain and loss of hearing. On examination a red or clear blister will be present on the ear drum. Treatment is antibiotics and rupturing the blister. Tympanic Membrane PerforationsTypically due to blunt trauma or direct penetrating trauma from Q-tips or other objects. Ciprodex antibiotic drops, and water precautions should be given, as well as ENT followup. Those with severe symptoms such as hearing loss, vertigo, or nystagmus should have urgent ENT followup. Otitis MediaOver 70% of OM is viral, but it is difficult to determine viral vs bacterial. Most bacterial infections are strep pneumo (50%). On exam the patient will have bulging of the TM or an air-fluid level. To accurately diagnose OM, you should be unable to move the TM with suction. Treatment is to either wait and watch or provide high-dose amoxicillin. Sudden Sensorineural Hearing LossAcute loss of hearing without an external or conductive cause. It is sudden (<72 hours) and unilateral, caused by viral, ischemic, or auto-immune causes. Syphilis and idiopathic intracranial hypertension can both cause acute unilateral hearing loss. Many cases are idiopathic. Treatment is either PO steroids or direct steroids to the middle ear, and urgent ENT followup. Antivirals should only be given if there are signs of a vesicular lesion. Bell's PalsyPatients presenting with symptoms of Bells Palsy should have a full history and physical examination to identify facial paralysis and possible causes, including evaluated for lesions of the TM concerning for Ramsay Hunt Syndrome. The AAO do not recommend routine lab testing or imaging in patients with Bell's Palsy, unless the patient lives in an area with endemic Lyme Disease. Patients should be treated with both oral antiviral AND oral steroid treatment together within 72 hours of symptom onset. Antiviral treatment alone is not recommended, however steroids alone may still have benefit. Patients should be sent home with eye protection and eye drops to prevent trauma and corneal abrasions or ulcers. AAO Guidelines.
CPR induced consciousness is characterized by a patient waking up, moving their limbs, or even fighting responders during compressions. Typically, when the providers stop compressions, either for a pulse check or because of assumed ROSC, the patient stops moving and again goes unresponsive. This has been described in both pre-hospital and hospital settings, and with improvement of CPR quality, will occur more frequently. What is CPR-Induced Consciousness?CPR Induced Consciousness occurs when CPR generates sufficient cerebral perfusion pressure (CPP) to allow for consciousness. CPP correlates closely with brain oxygenation. In 1995, the topic was first asked if patients should be sedated during CPR, but this was based off the idea that they patient may be conscious during the peri-arrest episode, not during the actual resuscitation itself. In a prospective study of 2060 victims of cardiac arrest, 46% of survivors reported memories of the CPR. Single images were placed on shelves visible to the patient to assess visual awareness during resuscitation, and all survivors were interviewed in a two step interview process. Most patients recalled themes of fear, bright light, violence or a sensation of being persecuted, seeing family, or recalling events that occured after ROSC. 2% actually recalled seeing and hearing actual events related to their resuscitation, including one episode that was verifiably accurate. (AWARE, S. Parnia et al. / Resuscitation 85 (2014) 1799–1805) A systematic review of case reports and published articles in 2015 found only 10 cases of actual awareness, excluding all near-death experiences, animal models, and non-purposeful movements. In 5 of 10 cases, CPR was initiated immediately and occured in-hospital. In all out-of-hospital cases, CPR began within 1-minute. All patients in the review had purposeful arm movements, while there was also a range of other findings including eye opening, localizing to painful stimuli, and even verbal communication, including adhering to instructions being given. A retrospective review of data from Victoria, Australia in 2017 found that CPR-Induced Consciousness is reported in approximately 0.7% of out-of-hospital cases, and increased over time from 2008 to 2014, presumptively from improvements in CPR quality. 87% of patients had body movement, 29% had vocalizations, and 20% had eye opening. Management of CPR Induced Consciousness: Due to higher-quality CPR, an unintended consequence has been CPR-induced consciousness, leading to some EMS agencies to creating protocols for sedation during CPR. These include IV or IM Ketamine (0.5-2mg) as well as midazolam. (Rice, 2016).
There is data showing that treating CPRIC is not associated with worsening outcomes or increased mortality, so you should consider treating CPRIC with either a small, repeated benzodiazapine or ketamine boluses. For treating Candida Vaginitis in early pregnancy, ACOG recommends local treatment instead of oral diflucan. This is based on studies that show higher doses (400-800 mg) of oral diflucan has been linked to birth defects. Although a 2013 NEJM cohort study found no association between diflucan and birth defects.
When treating pregnancy women for a UTI in early pregnancy, Nitrofurantoin or Bactrim are both not recommended as a first line agent. A Case-Control study published in 2009 showed an association between treatment with these medications in first trimester and malformations. While there are several limitations to this study, ACOG recommends avoiding these two medications in the first trimester. During the 2nd and 3rd trimester, sulfonamides and nitrofurantoin may be used as first-line therapy. Prescribing these in the first trimester is still considered appropriate when no other alternative is available. Penicillins, erythromycin, and cephalosporins have not been found to have any associations with birth defects. What is the differential diagnosis?
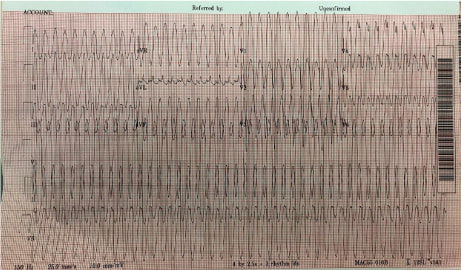
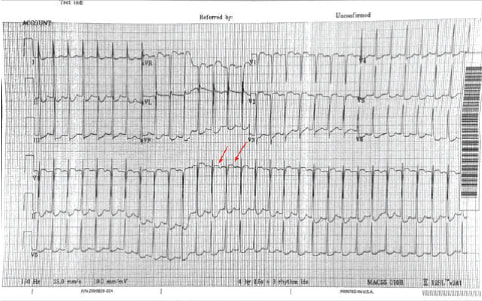
When approaching an EKG with tachycardia, one should first determine: is the QRS complex wide or narrow? And is the rhythm is regular or irregular? This patient’s EKG is regular with a wide QRS complex. Differential Diagnosis - Ventricular Tachycardia, SVT with Aberrancy (Bundle Branch Block or accessory pathway) or paced rhythm. No pacer spikes are seen which leaves VT and SVT with Aberrancy. A number of decision aid tools exist to assist in distinguishing (Brugada is most common) but are cumbersome. What's the final diagnosis?
Wide complex tachycardia likely Idiopathic Monomorphic VT originating from the RVOT. VT = QRS complexes originating in ventricle and > 30 second duration. < 30 second = NSVT. VT is classified as monomorphic (no beat to beat variation in QRS complex morphology) and polymorphic. VT can have ischemic or idiopathic etiologies. This 19 yo was unlikely to have ischemic heart disease. Management?
General Rule - Treat wide complex tachycardias as VT and cardioversion is always the safest option. Per ACLS STABLE patient with wide complex tachycardia that is REGULAR → an adenosine challenge can be attempted. This will terminate SVT and some Idiopathic VTs (eg RVOT). If unsuccessful ⇒ Procainamide Take home points:
1. Differing VT from SVT with aberrancy is not essential. It is always safest to treat as VT.
2. An adenosine challenge may be attempted for WCT only if the following two conditions are met: The patient is STABLE & The rhythm is REGULAR Sources: Link MS, Berkow LC, Kudenchuk PJ et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015; 132:S444 What is the diagnosis?
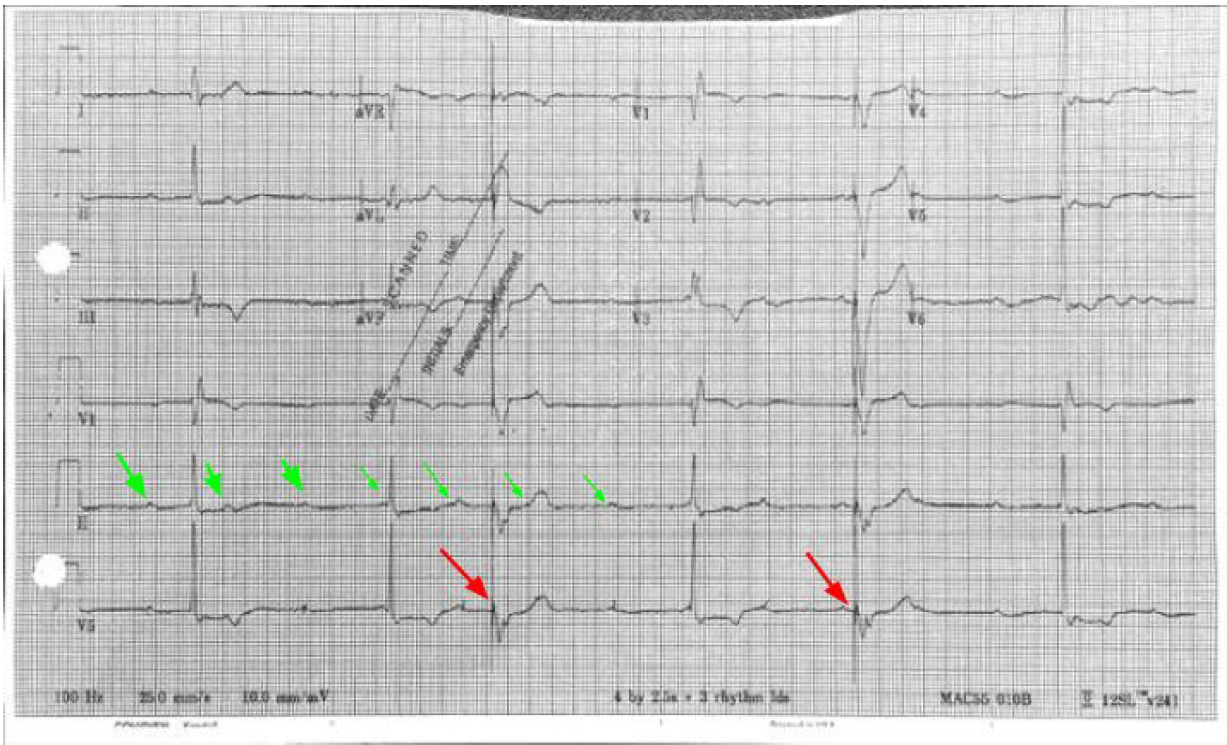
3rd Degree AV Block (Complete Heart Block) - Look at the rhythm strip and notice there is no relation between the P waves (Green Arrows) and QRS complexes which diagnoses 3rd Degree. It helps to get a piece of paper (calipers if you have) and measure the P waves. They can often be buried in the T wave or QRS complex. It is not 2nd Degree AV Block because both Mobitz I (progressively prolonged PR interval before dropped QRS) and Mobitz II (intermittent AV Block) will show some pattern of relation between the P wave and QRS complex. The escape rhythm is narrow and thus a junctional escape rhythm indicating the block is above the bundle of his. A wide complex would indicate a block at or below the bundle of His and ventricular escape rhythm. Name some possible etiologies
Etiologies: Ischemia (especially inferior MI), Medications (CCB, Beta blockers etc.) Hyperkalemia, and ask about travel and send a Lyme titer if pertinent or you’re feeling fancy **Look closely at the EKG you’ll see pacemaker spikes (Red Arrows) which are followed by ventricular capture. The patient had a PPM which had not been check in > 10 years and battery failure. Thus the pacemaker was not firing** What is the diagnosis?
This is a narrow complex regular tachycardia. The differential diagnosis includes - sinus tachycardia, atrial flutter, paroxysmal supraventricular tachycardia PSVT which includes AVNRT - AV nodal reentrant tachycardia and AVRT (Atrioventricular Reciprocating Tachycardia), atrial tachycardia, irregular narrow complex tachycardias would include MAT (Multifocal Atrial Tachycardia) and Atrial Fibrillation. The most commonly seen etiology is PSVT. There do not appear to be P waves. However it is difficult to definitively rule out the other etiologies. One must always consider Atrial Flutter with 2:1 block when the HR is around 150. Best lead to see P wave activity is V1 (here red arrows show some blips which may be buried Ps) Is there a role for adenosine?
Adenosine will frequently terminate a PSVT and unmask underlying atrial flutter so can often be diagnostic Name an initial non-pharmacologic intervention
Vagal maneuvers. Consider using a 10 cc syringe and asking the patient to blow the plunger out ( Lin ALiEM 2012 ). Additionally there may be improved success with vagal maneuvers using postural modification as described in the REVERT Trial ( Wiki EM Summary ) Take Home Points
1. Always consider Atrial Flutter with 2:1 conduction if the HR is around 150s
2. Adenosine can be therapeutic (terminating PSVT) and and diagnostic (unmasking P waves) 3. Consider postural modification to vagal maneuvers Resources: Lin,Michelle (2012,June26) https://www.aliem.com/2012/06/tricks-of-trade-valsalva-maneuver-by/ Brady WJ, Laughrey TS, Ghaemmaghami CA. Cardiac Rhythm Disturbances. In: Tintinalli JE, Stapcyznski JS, Ma OJ, Yealy DM, Meckler CD, Cline DM, editors. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 8th ed. McGraw-Hill; 2011. Appelboam A. et al. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial. Lancet 2015 Oct 31;386(10005):1747-53 Inhaled toxins frequently cause asphyxiation and can be classified further as chemical asphyxiants, simple asphyxiants, and pulmonary irritants.
Chemical Asphyxiants include Hydrogen Sulfide and cyanide. Hydrogen sulfide typically presents with a sulfur-like smell, while cyanide is typically presented in the burning of plastics. Simple Asphyxiants are anything which replaces oxygen in the atmosphere, including carbon monoxide or dioxide, methane, helium, or nitrogen. These may be present in a mine or other industrial setting, and may classically present as an unconscious worker who was attempting to rescue another unconscious worker. Irritant gases cause pulmonary irritation from coughing to diffuse lung injury. Irritants are categorized by their solubility; highly soluble irritants typically have strong scents because they are easily mixed into the upper airway, while less soluble irritants are typically less rapid in onset and will result in lower airway complaints.
Current Definitions
Blood CulturesUtilization of blood cultures can assist the treatment of many patients, however not every patient requires blood cultures. Whenever drawn, you should obtain two sets of cultures (or 3 for endocarditis). A recent article found a number needed to treat was 250 for a change in treatment, however other studies have found blood cultures more useful. Major Criteria:
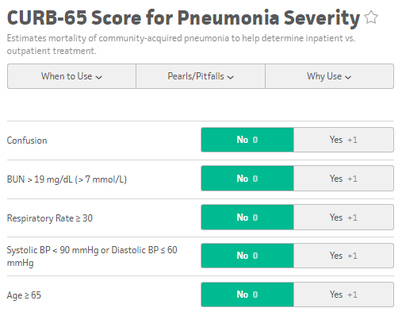
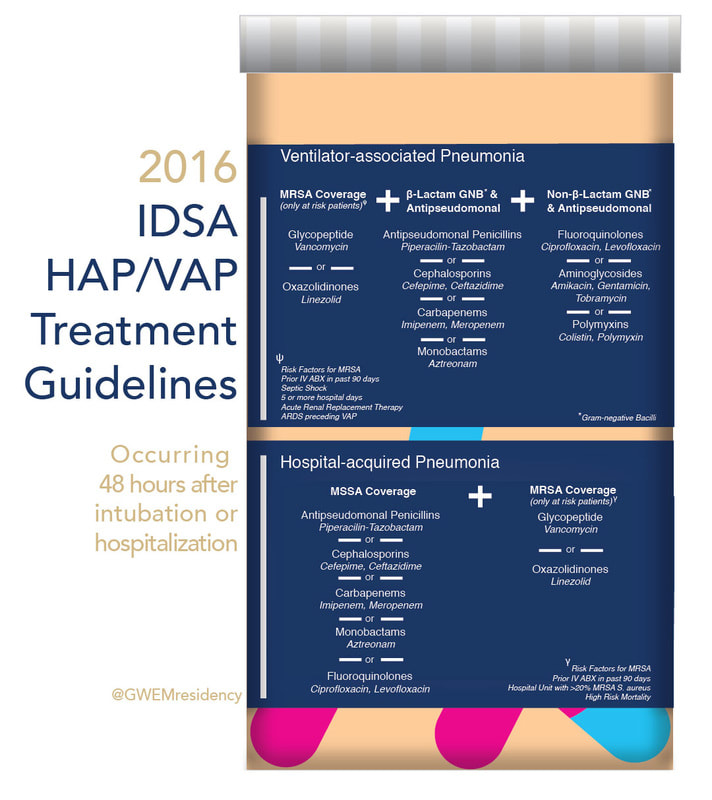
www.sciencedirect.com/science/article/pii/S0736467908004447?via%3DihubA blood culture is indicated by the rule if at least one major criterion or two minor criteria are present. Admission Criteria: CURB 65 and PSI/PORTPatients with CURB 65 scores 0-1 can potentially be discharged, however consider the patient's physical exam, oxygen saturation, and immunosupressed status, as the CURB 65 score does not take these into account. Those with a CURB 65 score greater than 3 should be considered for an ICU admission. The PSI/PORT score can also be used but is more thorough, including nursing home status, liver and heart disease status, as well as ABG data. While the CURB 65 has better specificity for identifying severe disease, the PSI/PORT score is more sensitive at identifying low-risk patients for discharge. TreatmentFor CAP, guidelines recommend Azithromycin or Doxycycline as azythromycin has increasing rates of resistance. In outpatients with co-morbidities or risk for resistance, you should consider levofloxacin or moxifloxacin. Patients admitted for CAP should be treated with single agent fluoroquinolone or dual agent treatment with ceftriaxone and azithromycin. ICU admitted CAP patients require an anti-pneumococcal betalactam (Ceftriaxone) and either azithromycin or fluoroquinolone. Treatment duration is typically 5 days.
|
Categories
Archive
February 2018
Please read our Terms of Use.
|
||||||||