|
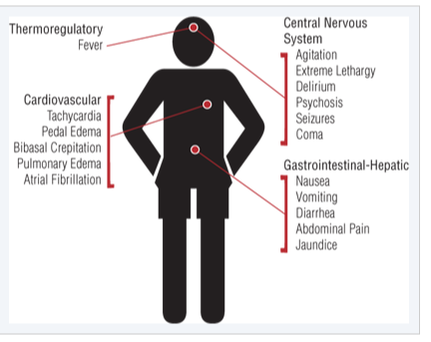
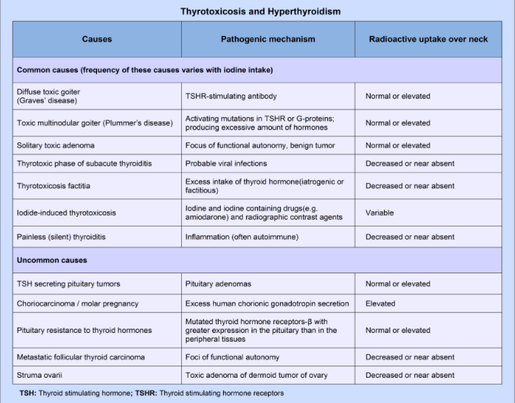
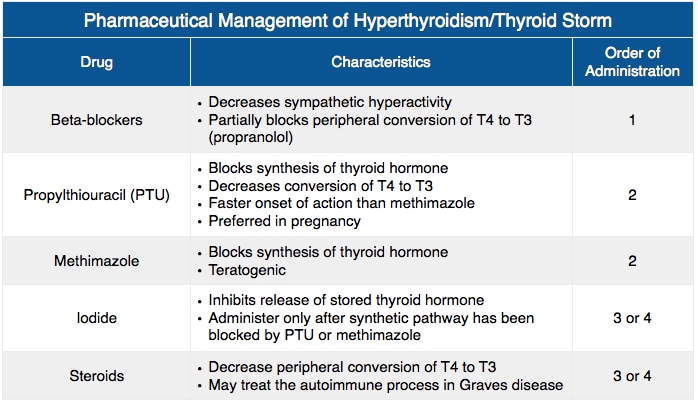
Thyroid hormone is frequently considered the 'thermostat' of the body, and affects many organ systems by increasing metabolic rate, heart rate, and muscle and nervous excitability. Thyroxine and triiodothyroxine are produced by the thyroid gland (T4, T3). T4 is the major hormone by a 20:1 ratio, but is peripherally converted to T3, which is significantly more potent than T4. Hyperthyroidism occurs when there is excess T4 or T3 circulating due to increased function of the gland itself (increased output, both primary or secondary). Primary hyperthyroidism is due to thyroid gland production, while secondary hyperthyroidism is due to excess production of TSH or TRH by the hypothalamic-pituitary axis. Thyrotoxicosis is when this hormone is from any other source; tumors or drug overdoses being most common. Thyroid storm is the most extreme presentation of excessive release of hormones or altered peripheral response to hormones, and carries an 80-100% mortality rate without treatment. Most commonly, thyroid storm is due to Graves Disease (85% of all thyroid storms) due to uncontrolled hormone secretion due to thyroidal receptor antibodies. Thyroid StormThe transition from thyrotoxicosis due to Graves Disease or other causes to thyroid storm is not fully understood. Adrenergic hyperactivity, either by increased hormone release or increased sensitivity plays a role in many of the symptoms, and patients with thyroid storm typically have higher thyroid hormone levels. Peripherally, T4 is converted to T3, which passes into the cellular nucleus and binds with the thyroid hormone receptor, as is typical for steroids. During thyroid storm, precipitants such as illness or stress will multiple the effect of thyroid hormones. Precipitants of a thyroid storm include infection, trauma, surgery, DKA or other medical illness. Additionally, patients undergoing antithyroid treatment may have thyroid storm secondary to withdrawal of the antithyroid drugs. PresentationPatients presenting with thyrotoxicosis or hyperthyroidism may have only vague constitutional symptoms such as weight loss or hair loss. Heat intolerance, anxiety, and palpitations are also classically associated with hyperthyroidism. On physical exam, goiters or neck masses may be present. Exophthalmos may be present, however cannot be used to judge the severity of the disease. Patients presenting with thyroid storm are typically agitated and may appear toxic. Fever can be quite high and common, as well as palpitations, shortness of breath, and hypertension secondary to increased contractility and cardiac output. Atrial fibrillation is present in 10-35% of cases. Diagnosis & TreatmentIn patients with a preexisting diagnosis of hyperthyroidism, thyroid storm is a clinical diagnosis based on your physical exam and history. Physicians should concentrate on evaluating temperature, cardiorespiratory, and neurologic (anxiety, agitation, seizure). The Buch & Wartofsky Scoring System is one method of scoring for thyroid storm, although I could find little data for its use since being published in 1993. In those without a known diagnosis, lab testing should include TSH, free T3/T4 levels, thyroid antibody titers, and any other lab testing as indicated. Further workup should be done to rule out infection as the precipitant of thyroid storm, including chest X-ray and urinalysis. EKG may show sinus tachycardia, and 10-35% of cases will have atrial fibrillation, however this is less likely in younger otherwise-healthy patients. Treatment of thyroid storm starts with supportive and symptomatic care, including ABCs, fluids, blood glucose stabilization. Thyroid hormone synthesis must then be inhibited using a Thionamide (methimazole or propylthiouracil PTU) to decrease the synthesis of hormones. Both medications are typically given PO with a single loading dose and then q4h doses afterwards. PTU has significant risks of hepatotoxicity, and the FDA recommends methimazole as first-line therapy. PTU is preferred only in pregnant patients during the first trimester. Once hormone synthesis is inhibited, hormone release should be stopped using potassium iodide, iodine lugol, or lithium carbonate. This can only occur 1 hour after PTU or methimazole therapy has been initiated. Finally, peripheral conversion of T4 to T3 should be inhibited using glucocorticoids such as hydrocortisone or dexamethasone. Glucocorticoid use has been shown to improve survival rates. Antibiotics should be considered if there are any signs of infection, as Thionamide medication can cause immune compromise during use, and thyroid storm patients are at risk for infection. Idrose A. Hyperthyroidism. In: Tintinalli JE, Stapczynski J, Ma O, Yealy DM, Meckler GD, Cline DM. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e. New York, NY: McGraw-Hill; 2016. http://accessmedicine.mhmedical.com.proxygw.wrlc.org/content.aspx?bookid=1658§ionid=109444027. Accessed February 05, 2017.
0 Comments
Leave a Reply. |
Categories
Archive
February 2018
Please read our Terms of Use.
|