|
In patients with bradycardias or cardiac arrest, have a high index of suspicion for hyperkalemia, especially in patients with renal failure or hemodialysis. Death from hyperkalemia is typically secondary to diastolic arrest or fibrillation, and common symptoms include weakness, paresthesias, and nausea/vomiting. Causes of Hyperkalemia
EKG Changes
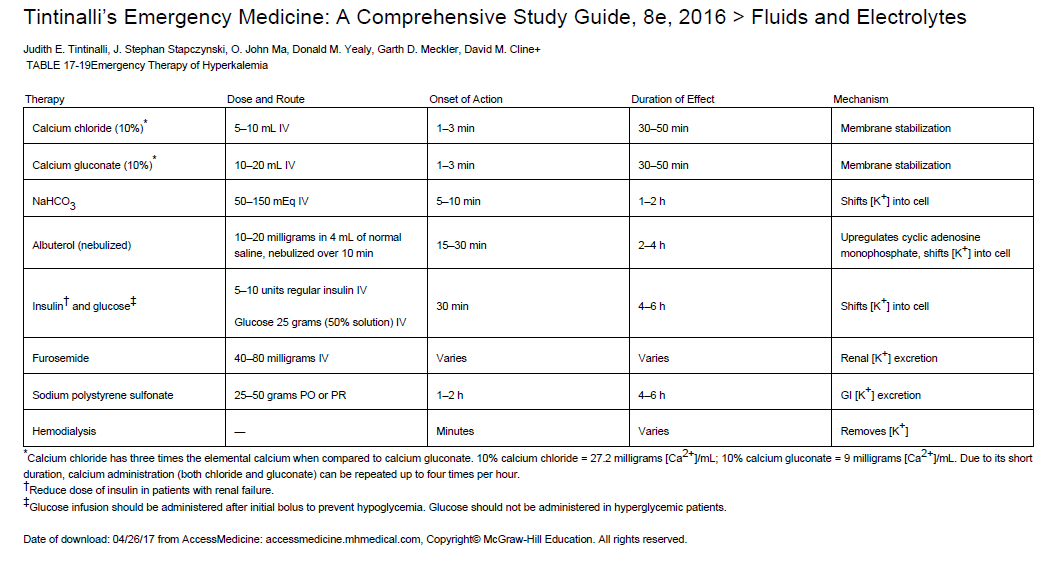
Treatment
0 Comments
Leave a Reply. |
Categories
Archive
February 2018
Please read our Terms of Use.
|
||||||