|
Adapted from Andy Simmon's Grand Rounds lecture, January 11th, 2017. How to identify serious injury that requires admisison for neurosurgery or observation, and how to instruct discharged patients for recovery expectations, followup, and return precautions. Classically, traumatic brain injury (TBI) is classified into mild, moderate, and severe. Mild TBI is considered concussion, while severe TBI has a mortality of 30% and less than 10% of severe TBIs experience full recovery.
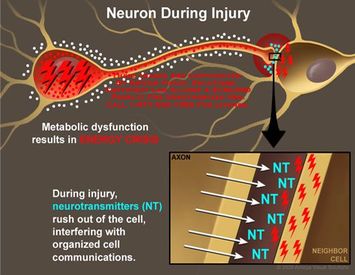
Alternative definitions include a discussion of impaired awareness or temporary change in brain status or neurologic function. ACEP states that concussions typically occur from nonpenetrating trauma to the head, presentation within 24 hours, and a GCS score of 14-15. Pathophysiology Disruption of the polarized neurons, leading to poor function. Efflux of potassium from the cell and influx of calcium into the cells leads to damage to mitochondria, disruption of neurotransmission, and damage of cells. Evaluation for Concussion
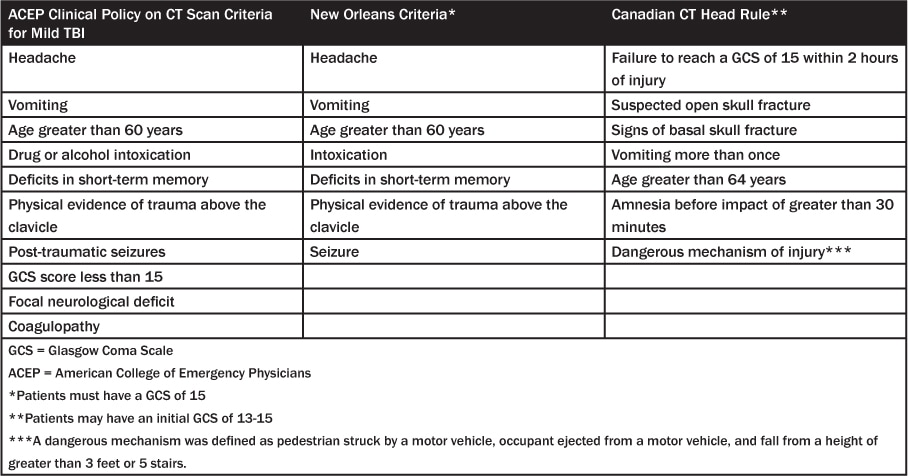
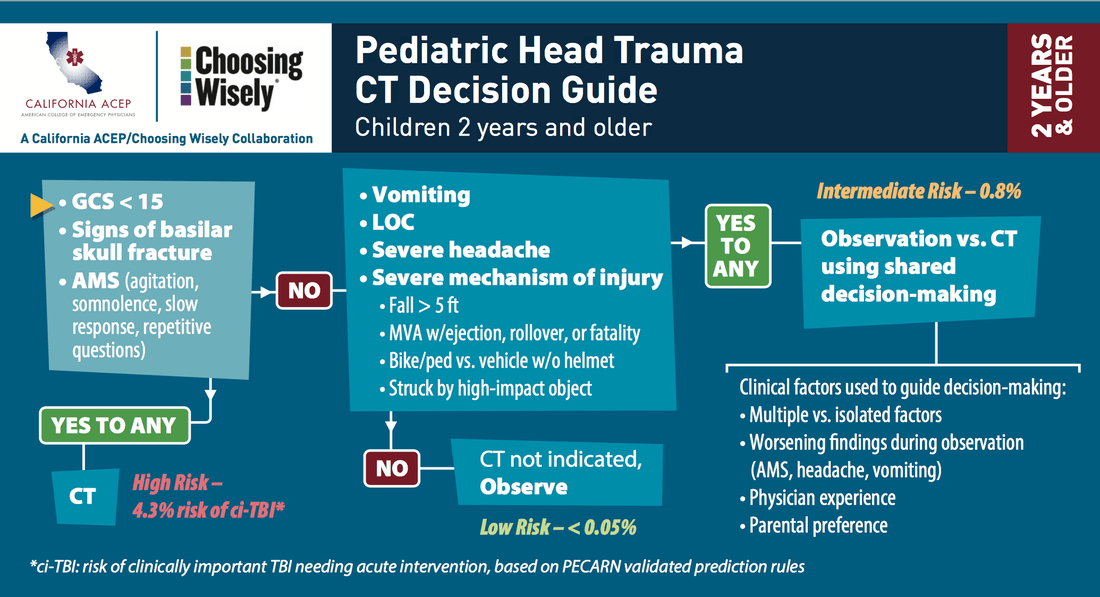
ManagementGoal is to identify those patients at risk for intracranial lesions, those who need observation, and those who may be discharged. Every patient should have a complete neurologic exam including gait and vestibulo-occular testing. VOMS testing (Vestibular/ocular motor screening) includes smooth pursuit, horizontal and vertical saccades, near point convergance, visual motion sensitivity, and horizontal vestibular ocular reflex. (Youtube howto). To help assess recovery expectations, these are some exams that can be used to assess injury. The R-WPTAS exam is the most commonly used. Neuroimaging should be determined by either the Canadian CT Head Rule or the New Orleans Criteria. Pediatric patients should be evaluated with the PECARN decision guidelines for imaging and observation. . Admission should be considered for patients with
Discharged patients should be counciled on instructions for recovery and treatment. Most guidelines instruct patients to rest for 3 days before attempting to return to daily activities. Patients should follow up with concussion clinic after 1 week, and not drive prior to re-evaluation. Every patient should be given a guideline for return to play or work.
9 Comments
12/26/2023 03:07:52 am
This Blog Is Very Helpful And Informative For This Particular Topic. I Appreciate Your Effort That Has Been Taken To Write This Blog For Us.Best hospital for brain stroke treatment in hyderabad, Recovery after brain stroke, Physiotherapy for brain stroke patient, Physiotherapy after brain stroke, Brain stem stroke rehabilitation, Brain stroke center in Hyderabad, Stroke brain damage recovery, Brain stem stroke recovery, Traumatic brain injury stroke recovery, Physiotherapy for brain stroke<a href="https://curerehab.in/Brain-Stroke-Rehabilitation"> physiotherapy in Hyderabad </a>
Reply
1/30/2024 02:45:08 am
This Blog Is Very Helpful And Informative For This Particular Topic. I Appreciate Your Effort That Has Been Taken To Write This Blog For Us.Best hospital for brain stroke treatment in hyderabad, Recovery after brain stroke, Physiotherapy for brain stroke patient, Physiotherapy after brain stroke, Brain stem stroke rehabilitation, Brain stroke center in Hyderabad, Stroke brain damage recovery, Brain stem stroke recovery, Traumatic brain injury stroke recovery, Physiotherapy for brain stroke<a href="https://curerehab.in/Brain-Stroke-Rehabilitation"> physiotherapy in Hyderabad </a>
Reply
2/5/2024 02:11:25 am
This Blog Is Very Helpful And Informative For This Particular Topic. I Appreciate Your Effort That Has Been Taken To Write This Blog For Us.Traumatic brain injury stroke recovery, traumatic brain injury rehabilitation, brain injury rehab, traumatic brain injury rehabilitation centers near me, brain injury rehabilitation near me, brain injury therapy, tbi physical therapy, traumatic brain injury clinic, traumatic brain injury care facilities, traumatic brain injury rehabilitation centers, traumatic brain injury rehab, brain injury treatment centers, rehab for brain injury near me, rehabilitation after brain injury<a href="https://curerehab.in/Traumatic-Brain-Injury-Rehabilitation"> physiotherapy in Hyderabad </a>
Reply
4/2/2024 02:46:37 am
This Blog Is Very Helpful And Informative For This Particular Topic. I Appreciate Your Effort That Has Been Taken To Write This Blog For Us.Traumatic brain injury stroke recovery, traumatic brain injury rehabilitation, brain injury rehab, traumatic brain injury rehabilitation centers near me, brain injury rehabilitation near me, brain injury therapy, tbi physical therapy, traumatic brain injury clinic, traumatic brain injury care facilities, traumatic brain injury rehabilitation centers, traumatic brain injury rehab, brain injury treatment centers, rehab for brain injury near me, rehabilitation after brain injury<a href="https://curerehab.in/Traumatic-Brain-Injury-Rehabilitation"> physiotherapy in Hyderabad </a>
Reply
4/20/2024 01:48:08 am
This Blog Is Very Helpful And Informative For This Particular Topic. I Appreciate Your Effort That Has Been Taken To Write This Blog For Us.Traumatic brain injury stroke recovery, traumatic brain injury rehabilitation, brain injury rehab, traumatic brain injury rehabilitation centers near me, brain injury rehabilitation near me, brain injury therapy, tbi physical therapy, traumatic brain injury clinic, traumatic brain injury care facilities, traumatic brain injury rehabilitation centers, traumatic brain injury rehab, brain injury treatment centers, rehab for brain injury near me, rehabilitation after brain injury<a href="https://curerehab.in/Traumatic-Brain-Injury-Rehabilitation"> physiotherapy in Hyderabad </a>
Reply
4/25/2024 09:56:15 pm
This Blog Is Very Helpful And Informative For This Particular Topic. I Appreciate Your Effort That Has Been Taken To Write This Blog For Us.Traumatic brain injury stroke recovery, traumatic brain injury rehabilitation, brain injury rehab, traumatic brain injury rehabilitation centers near me, brain injury rehabilitation near me, brain injury therapy, tbi physical therapy, traumatic brain injury clinic, traumatic brain injury care facilities, traumatic brain injury rehabilitation centers, traumatic brain injury rehab, brain injury treatment centers, rehab for brain injury near me, rehabilitation after brain injury<a href="https://curerehab.in/Traumatic-Brain-Injury-Rehabilitation"> physiotherapy in Hyderabad </a>
Reply
5/9/2024 06:10:49 am
This Blog Is Very Helpful And Informative For This Particular Topic. I Appreciate Your Effort That Has Been Taken To Write This Blog For Us.Traumatic brain injury stroke recovery, traumatic brain injury rehabilitation, brain injury rehab, traumatic brain injury rehabilitation centers near me, brain injury rehabilitation near me, brain injury therapy, tbi physical therapy, traumatic brain injury clinic, traumatic brain injury care facilities, traumatic brain injury rehabilitation centers, traumatic brain injury rehab, brain injury treatment centers, rehab for brain injury near me, rehabilitation after brain injury<a href="https://curerehab.in/Traumatic-Brain-Injury-Rehabilitation"> physiotherapy in Hyderabad </a>
Reply
5/17/2024 05:33:45 am
This Blog Is Very Helpful And Informative For This Particular Topic. I Appreciate Your Effort That Has Been Taken To Write This Blog For Us.Traumatic brain injury stroke recovery, traumatic brain injury rehabilitation, brain injury rehab, traumatic brain injury rehabilitation centers near me, brain injury rehabilitation near me, brain injury therapy, tbi physical therapy, traumatic brain injury clinic, traumatic brain injury care facilities, traumatic brain injury rehabilitation centers, traumatic brain injury rehab, brain injury treatment centers, rehab for brain injury near me, rehabilitation after brain injury<a href="https://curerehab.in/Traumatic-Brain-Injury-Rehabilitation"> physiotherapy in Hyderabad </a>
Reply
7/12/2024 01:31:40 am
This Blog Is Very Helpful And Informative For This Particular Topic. I Appreciate Your Effort That Has Been Taken To Write This Blog For Us.Traumatic brain injury stroke recovery, traumatic brain injury rehabilitation, brain injury rehab, traumatic brain injury rehabilitation centers near me, brain injury rehabilitation near me, brain injury therapy, tbi physical therapy, traumatic brain injury clinic, traumatic brain injury care facilities, traumatic brain injury rehabilitation centers, traumatic brain injury rehab, brain injury treatment centers, rehab for brain injury near me, rehabilitation after brain injury<a href="https://curerehab.in/Traumatic-Brain-Injury-Rehabilitation"> physiotherapy in Hyderabad </a>
Reply
Leave a Reply. |
Categories
Archive
February 2018
Please read our Terms of Use.
|
||||||||||||||