|
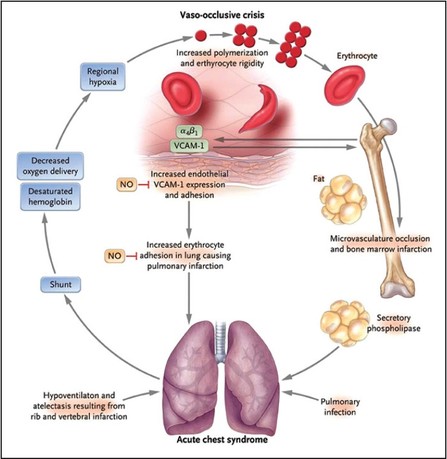
Adapted from Colton Hood's August 17th 2016 Grand Rounds lecture. One of the most common and severe complications of sickle cell disease, clinically may resemble a pneumonia, and can develop suddenly, and is more common in patients with asthma or those with prior acute chest events. Typically presents with cough, shortness of breath, and rales accompanied by a new infiltrate on chest X-ray. Mortality of acute chest syndrome is 9% in adults, and can lead to pulmonary hypertension, right heart failure, and risk of sudden death. Evaluate patients with sickle cell disease with acute onset of lower respiratory tract disease with or without fever for acute chest syndrome, including chest x-ray and pulse oximetry to measure oxygen saturation (NHLBI Consensus-Panel Expertise) Typically presents with sudden onset pain and;
Signs of severe acute chest syndrome event include:
Common causes of acute chest syndrome include:
Treatment of Acute Chest SyndromeEvaluate your sickle cell patients with labs, chest imaging, pain control and FEV. Be sure you are getting a chest X-ray and pulse-ox on any sickle cell patient complaining of chest pain. Incentive spirometry is strongly recommended and is associated with decreased rates of pulmonary complications.
Pain Control: See our Sickle Cell Pain Control Post
Be aware and prevent the following:
1 Comment
This Blog Is Very Helpful And Informative For This Particular Topic. I Appreciate Your Effort That Has Been Taken To Write This Blog For Us. Rehab after icu, intensive care syndrome, post intensive care unit, rehab care after surgery, rehabilitation after icu, post critical care unit, post critical care syndrome, critical care syndrome. <a href="https://curerehab.in/Post-ICU-Care"> physiotherapy in Hyderabad </a>
Reply
Leave a Reply. |
Categories
Archive
February 2018
Please read our Terms of Use.
|